Objectives: Mandibular condylar chondrocyte apoptosis is mainly responsible for the development and progression of temporomandibular joint osteoarthritis (TMJ-OA). Interleukin-1β (IL-1β) generally serves an agent that induces chondrocyte apoptosis. Hyperbaric oxygen (HBO) treatment increases proteoglycan synthesis in vivo. We explore the protective effect of HBO on IL-1β-induced mandibular condylar chondrocyte apoptosis in rats and the potential molecular mechanisms. Methods: Chondrocytes were isolated from the TMJ of 3-4-week old Sprague-Dawley rats. The Cell Counting Kit-8 (CCK-8) assay was used to determine cell viability. The phosphorylated phosphoinositide-3 kinase (p-PI3K), phosphorylated AKT (p-Akt), type II collagen (COL2), and aggrecan (AGG) content was detected by immunofluorescence, immunocytochemistry and western blotting. The expression of Pi3k, Akt, Col2 and Agg mRNA was measured using real-time quantitative polymerase chain reaction (RT-qPCR). Results: HBO inhibited the cytotoxicity and apoptosis induced by IL-1β (10 ng/mL) in the mandibular condylar chondrocytes. HBO also decreased the IL-1β activity that decreased p-PI3K and p-AKT levels, and increased COL2 and AGG expression, with the net effect of suppressing extracellular matrix degradation. Conclusions: These data suggest that HBO may protect mandibular condylar chondrocytes against IL-1β-induced apoptosis via the PI3K/AKT signaling pathway, and that it may promote the expression of mandibular condylar chondrocyte extracellular matrix through the PI3K/AKT signaling pathway.
Key Osteoarthritis Research
Hyperbaric oxygen treatment is comparable to acetylsalicylic acid treatment in an animal model of arthritis.
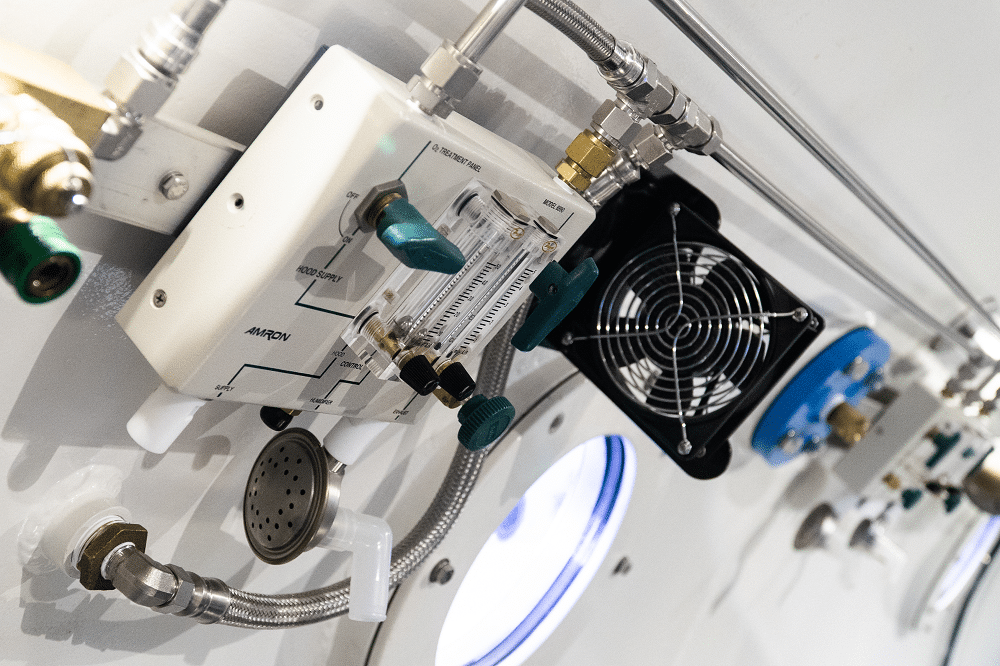
Approximately 1 in 5 adults in the United States are affected by the pain, disability, and decreased quality of life associated with arthritis. The primary focus of treatment is on reducing joint inflammation and pain through a variety of pharmacotherapies, each of which is associated with various side effects. Hyperbaric oxygen therapy is an alternative treatment that has been recommended to treat a variety of inflammatory diseases, ranging from chronic brain injury to exercise induced muscle soreness. The purpose of this set of experiments was to explore the effect of hyperbaric oxygen therapy on joint inflammation and mechanical hyperalgesia in an animal model of arthritis, and compare these effects to treatment with aspirin. Hyperbaric oxygen therapy significantly reduced both joint inflammation and hyperalgesia. As compared with aspirin treatment, hyperbaric treatment was equally as effective in decreasing joint inflammation and hyperalgesia. This article reports that hyperbaric oxygen treatment decreases pain and inflammation in an animal model of arthritis. The effect of hyperbaric oxygen treatment is very similar in magnitude to the effect of acetylsalicylic acid treatment. Potentially, hyperbaric oxygen could be used to treat pain and inflammation in patients with arthritis.