Post-COVID Syndrome
For some people, the effects of SARS-CoV-2, commonly referred to as COVID-19, extend past the 2-week acute-phase and into the months following initial infection. Those who continue to experience symptoms past the acute-phase are collectively being referred to as “COVID long-haulers,” and their numbers are quickly growing as the virus continues to spread. Long COVID is typically defined by persistent fatigue, shortness of breath, cognitive issues (e.g. brain fog), body aches, coughing, loss of taste and smell, and more that often result in an inability to return to normal levels of functioning (1).
Although the exact cause of long COVID is unclear, researchers believe that ongoing, low-grade inflammation in the brain may play a significant role(1). This helps explain why COVID long haulers experience symptoms such as fatigue, brain fog, and sensory issues as they are linked to issues of the central nervous system. Additionally, preliminary studies suggest that older individuals, women, and those with high BMIs may be at increased risk of experiencing long COVID(2,3). Therefore, therapies that decrease inflammation, such as hyperbaric oxygen therapy, IV therapy, and PEMF therapy may help alleviate symptoms of long COVID by effectively reducing neuroinflammation. Neurofeedback may provide relief of fatigue and brain fog by increasing activation in the brain.
Extivita Therapies for Chronic COVID Syndrome:
Extivita Therapies for Post-COVID Syndrome:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Listen to Laurie’s experience with Hyperbaric Oxygen Therapy to treat Post-Covid Syndrome
Hyperbaric Oxygen Therapy for Post-COVID Syndrome:
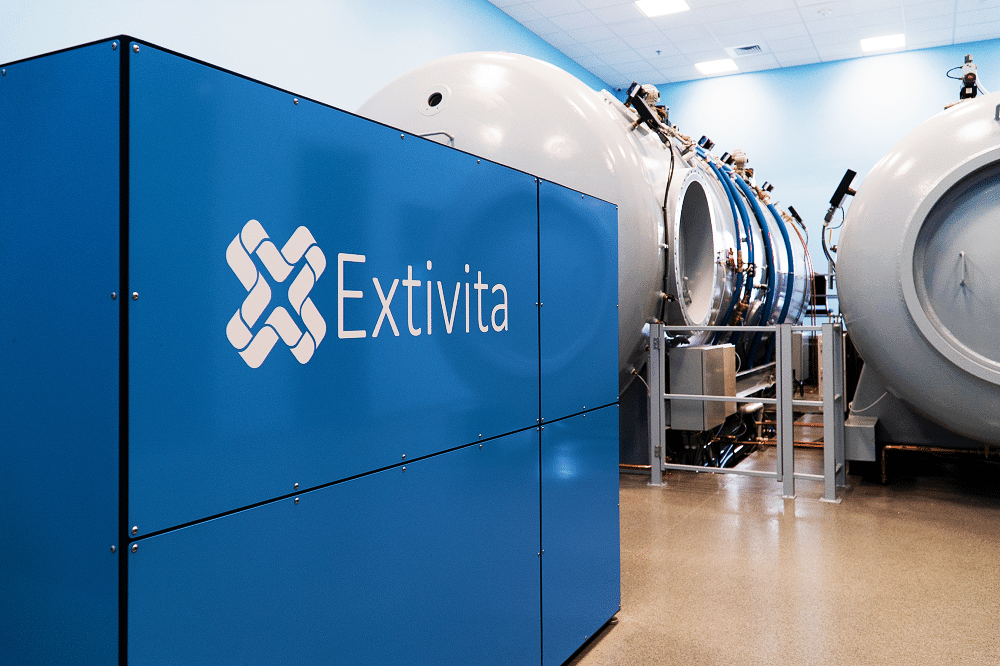
Hyperbaric oxygen therapy (HBOT) has the potential to improve the symptoms of long COVID due to its proven anti-inflammatory effects. HBOT has been shown to decrease inflammation by suppressing pro-inflammatory and increasing antioxidant gene expression(4-6). Additionally, studies on neurological conditions that involve inflammation (stroke, traumatic brain injury etc.) have found HBOT to have significant anti-inflammatory properties(7-9).
Because HBOT involves little to no risk given appropriate screening, we recommend its use to help reduce the symptoms of long COVID. Furthermore, our support of HBOT for long COVID is strengthened by the significant improvements that we have seen in patients who have already undergone HBOT for long COVID in our clinic.
Effects of HBOT on Post-COVID Syndrome:
New Blood Vessel Formation
Hyperbaric oxygen therapy stimulates the formation of new blood vessels, healing injured tissues that were unable to get nutrients and oxygen.
Increased Stem Cell Activity

Decreased Inflammation

Neurofeedback for Post-COVID Syndrome:
Neurofeedback may not target the root cause of long COVID, but it can improve symptoms of fatigue and brain fog by increasing general brain activation. A review of neurofeedback research revealed reduced ratings of fatigue and improved cognition across several different disorders(10). Neurofeedback protocols for long COVID are developed based on the individual’s EEG brain map, behavioral symptoms, and neurofeedback consultation, but will typically involve reducing slow wave activity that may be suppressing brain activation.
IV Therapy for Post-COVID Syndrome:
We strongly recommend both our Myer’s Cocktail IV and glutathione IV for those experiencing long COVID due to their scientifically proven anti-inflammatory effects. Depletions in magnesium, vitamins B3, B6, and biotin (part of the B-complex), all of which are in the Myer’s cocktail IV, have been associated with increased inflammation(11-13). Vitamin C, also included in the Myer’s IV, is known to have beneficial effects on the immune system and increased inflammation. Vitamin C has been shown to 1) inhibit excessive, damaging inflammation 2) reduce levels of free radicals (and therefore prevent the associated inflammation), and 3) decrease levels of pro-inflammatory markers themselves(14-16). Increasing levels of these vitamins via the Myer’s IV may help reduce symptoms of long COVID by decreasing inflammation.
Glutathione, which is considered the “master antioxidant,” plays a vital role in maintaining strong immune function and reducing oxidative stress, which often leads to inflammation(17-18). It also has demonstrated antiviral properties by decreasing viral load and the ensuing “inflammatory cascade,” something that is of huge concern regarding COVID severity(19). Given the several immune-related benefits of glutathione, we suggest that those suffering from long COVID may find relief from intravenous glutathione IV’s.

Pulsed Electromagnetic Field Therapy for Post-COVID Syndrome:
Pulsed-electromagnetic field therapy (PEMF) is a vascular therapy designed to optimize blood flow throughout the entire body by enhancing the microcirculation, the circulatory functioning of our smallest blood vessels. PEMF may help alleviate the symptoms of long COVID by decreasing the harmful inflammatory cascade that may be implicated in long COVID(20). When used on its own, or in conjunction with HBOT and IV therapy, PEMF can be a powerful therapy to help with symptoms of long COVID.
News & Research for Post-COVID Syndrome:
US Navy Honors Hyperbaric Medicine Physician for Treating Covid Long-Haulers
Greenwich Hospital’s Sandra Wainwright, MD, a self-described military brat and medical director of the Center for Hyperbaric Medicine and Wound Healing, was commended by the U.S. Navy on Monday for treating a sailor with debilitating long-haul symptoms of COVID-19....
Ask the Doctors: HBOT a potential treatment for long COVID-19
Dear Doctors: I got COVID-19, which wasn’t too bad. But now I’ve got long COVID. I’m exhausted all the time, my heart races and I’ve got brain fog. It’s derailing my life. I saw on the news that the method for treating scuba divers with the bends works for long COVID....
‘OxyGeneration chamber in Galway being used to treat long Covid’
Image from CLARE ECHO article It’s over a century since hyperbaric oxygen therapy treatment (HBOT) first gained prominence. Treatment for illness caused by deep-sea diving was the first port of call for HBOT and later aiding the healing of wounds during wartime. The...
References
- Baig, Abdul Mannan. “Deleterious Outcomes in Long-Hauler COVID-19: The Effects of SARS-CoV-2 on the CNS in Chronic COVID Syndrome.” ACS Chemical Neuroscience, vol. 11, no. 24, Dec. 2020, pp. 4017–20. PubMed Central, doi:10.1021/acschemneuro.0c00725.
- Sudre, Carole H., et al. “Attributes and Predictors of Long-COVID: Analysis of COVID Cases and Their Symptoms Collected by the Covid Symptoms Study App.” MedRxiv, Cold Spring Harbor Laboratory Press, Oct. 2020, p. 2020.10.19.20214494. www.medrxiv.org, doi:10.1101/2020.10.19.20214494.
- Townsend, Liam, et al. “Persistent Fatigue Following SARS-CoV-2 Infection Is Common and Independent of Severity of Initial Infection.” PLOS ONE, vol. 15, no. 11, Public Library of Science, Nov. 2020, p. e0240784. PLoS Journals, doi:10.1371/journal.pone.0240784.
- Benson, R. M., et al. “Hyperbaric Oxygen Inhibits Stimulus-Induced Proinflammatory Cytokine Synthesis by Human Blood-Derived Monocyte-Macrophages.” Clinical and Experimental Immunology, vol. 134, no. 1, Oct. 2003, pp. 57–62. PubMed Central, doi:10.1046/j.1365-2249.2003.02248.x.
- Lin, Kao-Chang, et al. “Attenuating Inflammation but Stimulating Both Angiogenesis and Neurogenesis Using Hyperbaric Oxygen in Rats with Traumatic Brain Injury.” The Journal of Trauma and Acute Care Surgery, vol. 72, no. 3, Mar. 2012, pp. 650–59. PubMed, doi:10.1097/TA.0b013e31823c575f.
- Godman, Cassandra A., et al. “Hyperbaric Oxygen Treatment Induces Antioxidant Gene Expression.” Annals of the New York Academy of Sciences, vol. 1197, June 2010, pp. 178–83. PubMed, doi:10.1111/j.1749-6632.2009.05393.x.
- Shapira, Ronit, et al. “Hyperbaric Oxygen Therapy Ameliorates Pathophysiology of 3xTg-AD Mouse Model by Attenuating Neuroinflammation.” Neurobiology of Aging, vol. 62, Feb. 2018, pp. 105–19. ScienceDirect, doi:10.1016/j.neurobiolaging.2017.10.007.
- Geng, Fengyang, et al. “Effects of Hyperbaric Oxygen Therapy on Inflammasome Signaling after Traumatic Brain Injury.” Neuroimmunomodulation, vol. 23, no. 2, Karger Publishers, 2016, pp. 122–29. www.karger.com, doi:10.1159/000445689.
- Vlodavsky, E., et al. “Hyperbaric Oxygen Therapy Reduces Neuroinflammation and Expression of Matrix Metalloproteinase-9 in the Rat Model of Traumatic Brain Injury.” Neuropathology and Applied Neurobiology, vol. 32, no. 1, 2006, pp. 40–50. Wiley Online Library, doi:https://doi.org/10.1111/j.1365-2990.2005.00698.x.
- Luctkar-Flude, Marian, and Dianne Groll. “A Systematic Review of the Safety and Effect of Neurofeedback on Fatigue and Cognition.” Integrative Cancer Therapies, vol. 14, no. 4, SAGE Publications Inc STM, July 2015, pp. 318–40. SAGE Journals, doi:10.1177/1534735415572886.
- Nielsen, Forrest H. “Effects of Magnesium Depletion on Inflammation in Chronic Disease.” Current Opinion in Clinical Nutrition and Metabolic Care, vol. 17, no. 6, Nov. 2014, pp. 525–30. PubMed, doi:10.1097/MCO.0000000000000093.
- Kennedy, David O. “B Vitamins and the Brain: Mechanisms, Dose and Efficacy—A Review.” Nutrients, vol. 8, no. 2, Jan. 2016. PubMed Central, doi:10.3390/nu8020068.
- Vitamin B-6 Intake Is Inversely Related to, and the Requirement Is Affected by, Inflammation Status – PubMed. https://pubmed.ncbi.nlm.nih.gov/19906811/. Accessed 9 Feb. 2021.
- Holmannová, D., et al. “[Vitamin C and its physiological role with respect to the components of the immune system].” Vnitrni Lekarstvi, vol. 58, no. 10, Oct. 2012, pp. 743–49.
- Wannamethee, S. Goya, et al. “Associations of Vitamin C Status, Fruit and Vegetable Intakes, and Markers of Inflammation and Hemostasis.” The American Journal of Clinical Nutrition, vol. 83, no. 3, Mar. 2006, pp. 567–74; quiz 726–27. PubMed, doi:10.1093/ajcn.83.3.567.
- Ellulu, Mohammed S., et al. “Effect of Vitamin C on Inflammation and Metabolic Markers in Hypertensive and/or Diabetic Obese Adults: A Randomized Controlled Trial.” Drug Design, Development and Therapy, vol. 9, July 2015, pp. 3405–12. PubMed Central, doi:10.2147/DDDT.S83144.
- Alpert, Michelle. “The Diverse Benefits of Glutathione: A Key Antioxidant for Reversing Chronic Illness.” Alternative and Complementary Therapies, vol. 11, no. 5, Oct. 2005, pp. 241–45. DOI.org (Crossref), doi:10.1089/act.2005.11.241.
- Forman, Henry Jay, et al. “Glutathione: Overview of Its Protective Roles, Measurement, and Biosynthesis.” Molecular Aspects of Medicine, vol. 30, no. 1–2, Apr. 2009, pp. 1–12. PubMed, doi:10.1016/j.mam.2008.08.006.
- Polonikov, Alexey. “Endogenous Deficiency of Glutathione as the Most Likely Cause of Serious Manifestations and Death in COVID-19 Patients.” ACS Infectious Diseases, May 2020. PubMed Central, doi:10.1021/acsinfecdis.0c00288.
- Wade, Brett. “A Review of Pulsed Electromagnetic Field (PEMF) Mechanisms at a Cellular Level: A Rationale for Clinical Use.” American Journal of Health Research, vol. 1, no. 3, 3, Science Publishing Group, Jan. 2014, p. 51. www.sciencepublishinggroup.com, doi:10.11648/j.ajhr.20130103.13.




