Spinal Cord Injuries
An estimated 291,000 persons live with a spinal cord injury (SCI), with roughly 17,730 new cases occurring each year(1). Current research and treatments focus on reducing the “secondary injury cascade” that begins immediately after the initial spinal cord trauma(2). This cascade occurs during either the sub-acute (weeks to months after initial injury) or chronic phase (months to years after initial injury), or during both (3). The severity of this secondary damage directly impacts further bodily damage and the restorative process.
Fortunately, research has shown a correlation between reduced secondary damage and improved neurological outcomes(4, 5). Therapies that can reduce the severity of the secondary injury cascade, such as hyperbaric oxygen therapy, have the potential to reduce the cellular damage that occurs post-injury, and therefore improve neurological outcomes.
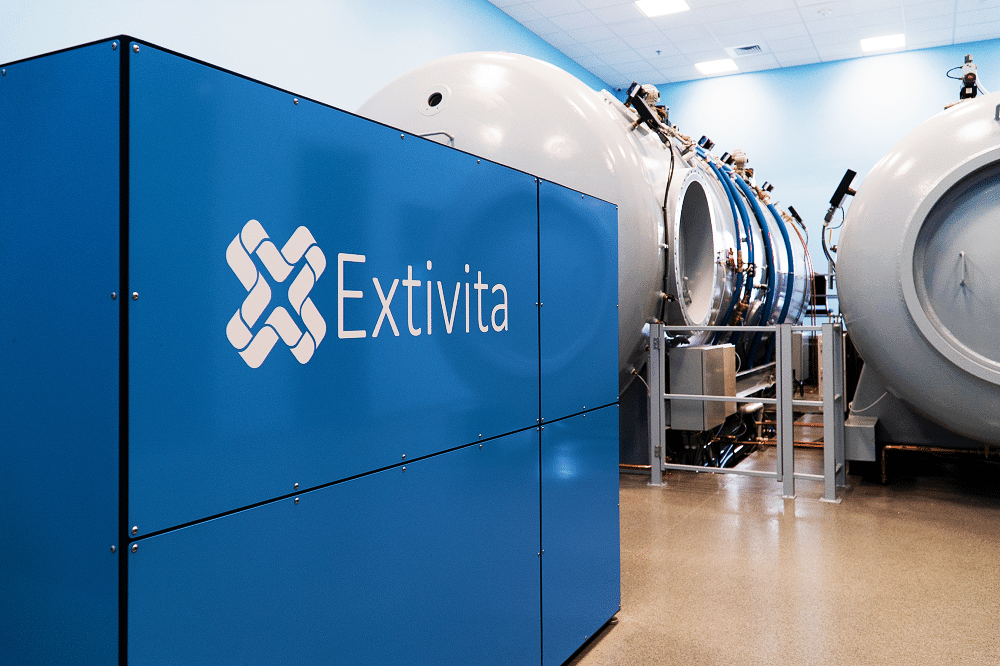
Extivita Therapies for Spinal Cord Injuries:
Extivita Therapies Spinal Cord Injury Recovery:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Ryley’s experience with
Hyperbaric Oxygen Therapy
to treat his
Spinal Cord Injury
Hyperbaric Oxygen Therapy for Spinal Cord Injury:
Hyperbaric Oxygen Therapy (HBOT) increases oxygen to the damaged spinal cord tissue, thereby decreasing the cell death and damage that can occur for weeks to months after initial injury (6, 7). Additionally, HBOT decreases spinal cord edema (swelling) and inflammation(3) and has been shown to reduce synaptic and dendritic degeneration in animal models(8).
Synaptic and dendritic degeneration refers to the degradation of connections between nerve cells, which are essential for healthy neurological function. Reducing such degeneration via HBOT may preserve connections in the spinal cord and brain and thus decrease the severity of neurological impairment.
HBOT Research Shows Improvement To:
- Reduces cell death
- Reduces inflammation and swelling
- Reduces oxidative stress
Effects of HBOT on Spinal Cord Injury:

Decreased Inflammation
New Blood Vessel Formation
Increased Stem Cell Activity

Neurofeedback for Spinal Cord Injury:
Neurofeedback may help relieve the central neuropathic pain (CNP) that 50% of SCI patients experience(9-10). CNP is characterized by burning, aching, and prickling sensations that often lead to anxiety and sleep issues, as well as a lower quality of life(9, 11-12). There is some evidence that neurofeedback therapy can reduce ratings of pain in SCI patients with CNP. One study found that 80% of study participants experienced statistically significant pain reduction following sessions of alpha reward training(10). Given this, we recommend neurofeedback therapy for people with SCI who may not be responding to traditional CNP treatment, and for those looking for an alternative method of pain relief.
IV Therapy for Spinal Cord Injury:
Nutritional IV therapy has strong potential to limit that damage of the secondary injury cascade that occurs post-SCI. A hallmark of the secondary phase of SCI is oxidative stress, which occurs when levels of reactive oxygen and/or nitrogen species are elevated(13-14). Brain cells are particularly susceptible to damage from oxidative stress, but such damage can be reduced by improving antioxidant defenses(15).
We recommend our NAD+ IV trio for people with SCI. This trio includes NAD+, a Myer’s Cocktail IV, and a glutathione IV. Both the Myer’s Cocktail IV and glutathione IV have powerful antioxidant effects that may reduce the secondary injury cascade by combating oxidative stress(16-17). The NAD+ can also provide benefits for SCI by improving mitochondrial function, which is impaired in those with SCI(13, 18).


Pulsed Electromagnetic Field Therapy for Spinal Cord Injury:
There is some evidence to suggest that pulsed electromagnetic field (PEMF) therapy may promote functional recovery and reduce the secondary injury cascade in those with SCI. These benefits are likely due to PEMF’s ability to reduce inflammation and oxidative stress, both of which are involved in the secondary injury phase of SCI(19).
News & Research for Spinal Cord Injury:
Hyperbaric oxygen therapy reduces apoptosis and dendritic/synaptic degeneration via the BDNF/TrkB signaling pathways in SCI rats
Abstract Spinal cord injury (SCI) is a serious neurological disease without efficacious drugs. Anti-apoptosis and suppressing dendritic/synaptic degeneration in the anterior horn are essential targets after SCI. Previous studies found that hyperbaric oxygen therapy...
Role of Hyperbaric Oxygen Therapy in Trauma Care
Article from Bio Spectrum Media discusses how technological advancements have made the use of HBOT more efficient in Trauma Care: Head Trauma is one of the major causes of death and disabilities across the world. This can be caused due a contusion (bruise),...
Evaluation of hyperbaric oxygen therapy for spinal cord injury in rats with different treatment course using diffusion tensor imaging.
Animal study. To evaluate the efficacy of hyperbaric oxygen (HBO) therapy for spinal cord injury (SCI) in rats with different treatment course using diffusion tensor imaging (DTI). Hospital in Fuzhou, China. Fifty adult Sprague-Dawley rats were grouped as: (A) sham-operated group (n = 10); (B) SCI without HBO therapy group (n = 10); (C) SCI with HBO therapy for 2 weeks (SCI+HBO) group (n = 10); (D) SCI with HBO therapy for 4 weeks (SCI+HBO) group (n = 10); (E) SCI with HBO therapy for 6 weeks (SCI+HBO) group (n = 10). Basso Beattie Bresnahan (BBB) scores and diffusion tensor imaging parameters including fractional anisotropy (FA), mean diffusivity (MD), radial diffusion (RD), and axial diffusion (AD) values in the injury epicenter, as well as 2 mm rostral and caudal to the injury epicenter were collected and analyzed 6 weeks post-injury.
References
- “Home Page – NSCISC Application.” Accessed June 19, 2019. https://www.nscisc.uab.edu/.
- “Spinal Cord Injury Information: Levels, Causes, Recovery.” Accessed June 19, 2019. https://www.shepherd.org/patient-programs/spinal-cord-injury/about#FAQ3.
- Oyinbo, Charles Aidemise. “Secondary Injury Mechanisms in Traumatic Spinal Cord Injury: A Nugget of This Multiply Cascade.” Acta Neurobiologiae Experimentalis 71, no. 2 (2011): 281–99. https://pdfs.semanticscholar.org/8131/2216495186e1d35f6958c59587714efca557.pdf
- Dumont, R. J., D. O. Okonkwo, S. Verma, R. J. Hurlbert, P. T. Boulos, D. B. Ellegala, and A. S. Dumont. “Acute Spinal Cord Injury, Part I: Pathophysiologic Mechanisms.” Clinical Neuropharmacology 24, no. 5 (October 2001): 254–64. https://www.ncbi.nlm.nih.gov/pubmed/11586110
- Kwon, Brian K., Wolfram Tetzlaff, Jonathan N. Grauer, John Beiner, and Alexander R. Vaccaro. “Pathophysiology and Pharmacologic Treatment of Acute Spinal Cord Injury.” The Spine Journal 4, no. 4 (July 1, 2004): 451–64. https://doi.org/10.1016/j.spinee.2003.07.007
- Kelly, D. L., K. R. Lassiter, A. Vongsvivut, and J. M. Smith. “Effects of Hyperbaric Oxygenation and Tissue Oxygen Studies in Experimental Paraplegia.” Journal of Neurosurgery 36, no. 4 (April 1972): 425–29. https://doi.org/10.3171/jns.1972.36.4.0425.
- Emery, E., P. Aldana, M. B. Bunge, W. Puckett, A. Srinivasan, R. W. Keane, J. Bethea, and A. D. Levi. “Apoptosis after Traumatic Human Spinal Cord Injury.” Journal of Neurosurgery 89, no. 6 (December 1998): 911–20. https://doi.org/10.3171/jns.1998.89.6.0911.
- Ying, Xinwang, Wenzhan Tu, Sisi Li, Qiaoyun Wu, Xiaolong Chen, Ye Zhou, Jie Hu, Guanhu Yang, and Songhe Jiang. “Hyperbaric Oxygen Therapy Reduces Apoptosis and Dendritic/Synaptic Degeneration via the BDNF/TrkB Signaling Pathways in SCI Rats.” Life Sciences 229 (July 15, 2019): 187–99. https://doi.org/10.1016/j.lfs.2019.05.029.
- Siddall, Philip J., et al. “A Longitudinal Study of the Prevalence and Characteristics of Pain in the First 5 Years Following Spinal Cord Injury.” Pain, vol. 103, no. 3, June 2003, pp. 249–57. ScienceDirect, doi:10.1016/S0304-3959(02)00452-9.
- Vučković, Aleksandra, et al. “EEG Correlates of Self-Managed Neurofeedback Treatment of Central Neuropathic Pain in Chronic Spinal Cord Injury.” Frontiers in Neuroscience, vol. 13, Frontiers, 2019. Frontiers, doi:10.3389/fnins.2019.00762.
- Finnerup, Nanna B., et al. “Neuropathic Pain Clinical Trials: Factors Associated with Decreases in Estimated Drug Efficacy.” Pain, vol. 159, no. 11, Nov. 2018, pp. 2339–46. PubMed Central, doi:10.1097/j.pain.0000000000001340.
- Middleton, James, et al. “Relationship Between Quality of Life and Self-Efficacy in Persons With Spinal Cord Injuries.” Archives of Physical Medicine and Rehabilitation, vol. 88, no. 12, Dec. 2007, pp. 1643–48. ScienceDirect, doi:10.1016/j.apmr.2007.09.001.
- Azbill, Robert D., et al. “Impaired Mitochondrial Function, Oxidative Stress and Altered Antioxidant Enzyme Activities Following Traumatic Spinal Cord Injury.” Brain Research, vol. 765, no. 2, Aug. 1997, pp. 283–90. ScienceDirect, doi:10.1016/S0006-8993(97)00573-8.
- Pizzino, Gabriele, et al. “Oxidative Stress: Harms and Benefits for Human Health.” Oxidative Medicine and Cellular Longevity, vol. 2017, 2017. PubMed Central, doi:10.1155/2017/8416763.
- Jia, Z., et al. “Oxidative Stress in Spinal Cord Injury and Antioxidant-Based Intervention.” Spinal Cord, vol. 50, no. 4, 4, Nature Publishing Group, Apr. 2012, pp. 264–74. www.nature.com, doi:10.1038/sc.2011.111.
- Carr, Anitra C., and Silvia Maggini. “Vitamin C and Immune Function.” Nutrients, vol. 9, no. 11, Nov. 2017. PubMed Central, doi:10.3390/nu9111211.
- Forman, Henry Jay, et al. “Glutathione: Overview of Its Protective Roles, Measurement, and Biosynthesis.” Molecular Aspects of Medicine, vol. 30, no. 1–2, Apr. 2009, pp. 1–12. PubMed, doi:10.1016/j.mam.2008.08.006.
- Johnson, Sean, and Shin-ichiro Imai. “NAD + Biosynthesis, Aging, and Disease.” F1000Research, vol. 7, Feb. 2018. PubMed Central, doi:10.12688/f1000research.12120.1.
- Wang, Chunyan, et al. “Lowfrequency Pulsed Electromagnetic Field Promotes Functional Recovery, Reduces Inflammation and Oxidative Stress, and Enhances HSP70 Expression Following Spinal Cord Injury.” Molecular Medicine Reports, vol. 19, no. 3, Spandidos Publications, Mar. 2019, pp. 1687–93. www.spandidos-publications.com, doi:10.3892/mmr.2019.9820.



