Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) is characterized by chronic inflammation of the gastrointestinal (GI) tract. Crohn’s disease and ulcerative colitis are the two most prevalent IBD conditions, and both are likely caused by a mix of genetic and environmental factors that result in issues with the immune response (1). IBD patients have consistently displayed higher levels of proinflammatory cytokines (2) as well as nitric oxide, both of which can lead to tissue damage (3).
Extivita Therapies for IBD:
Extivita Therapies IBD Recovery:
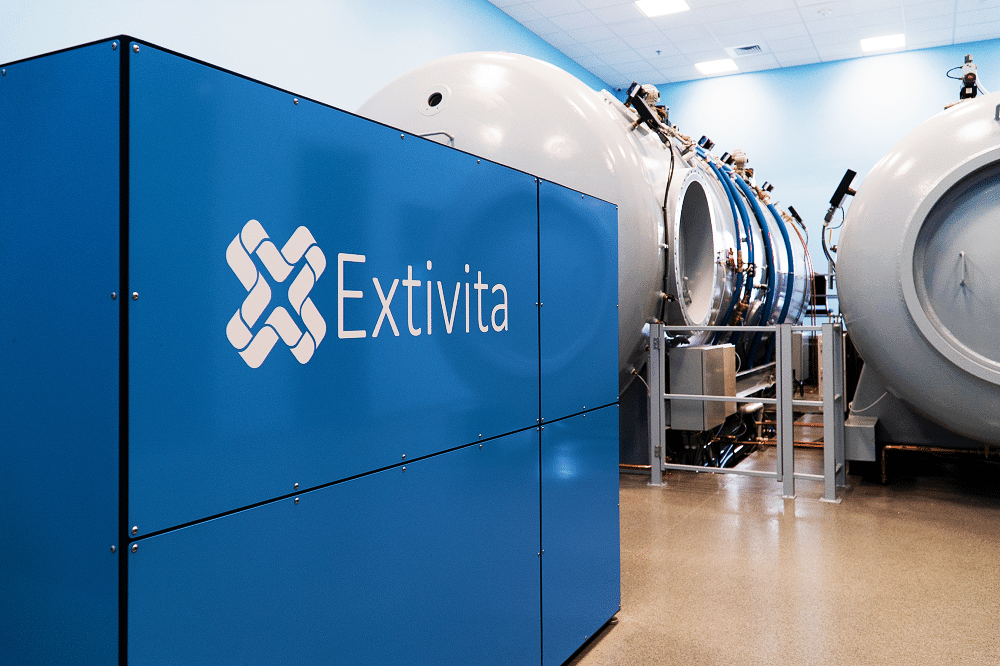
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Listen to Bryce’s experience with Hyperbaric Oxygen Therapy to treat Ulcerative Colitis
Hyperbaric Oxygen Therapy for Inflammatory Bowel Disease:
See the page on Crohn’s Disease and the page on Ulcerative Colitis for more information.
Effects of HBOT on Inflammatory Bowel Disease:

Decreased Inflammation
Increased Stem Cell Activity
New Blood Vessel Formation
Hyperbaric oxygen therapy stimulates the formation of new blood vessels, healing injured tissues that were unable to get nutrients and oxygen.

Neurofeedback for Inflammatory Bowel Disease:
There is scientific evidence showing the intimate connection between the gut and the brain, and the effect of this shared interaction on gut and psychological well-being. Patients with IBD may benefit from integration of mind and body interventions which may help decrease triggers such as stress and anxiety (6). Neurofeedback is a type of biofeedback which may be helpful in treating symptoms of IBD by calming the nervous system.
IV Therapy for Inflammatory Bowel Disease:
Patients with IBD are at risk for nutrient deficiencies because of reduced dietary intake, inflammation, and the underlying malabsorption (7). Antioxidant depletion can result from dealing with oxidative stress from inflammation occurring in IBD (9). Myers’ cocktail is a form of nutrient therapy which contains vitamin C, magnesium, B12, B6, B5, B complex, and calcium given intravenously (through the veins) (8) . This process bypasses the digestive system and a much higher level of nutrients and antioxidants is directly delivered to your cells. Myers’ cocktail and glutathione are safe and effective adjunctive treatments for IBD.


Pulsed Electromagnetic Field Therapy for IBD:
According to studies, the microcirculation and inside lining of the blood vessels play a critical role in body’s immune balance. In IBD, micro vessels in chronically inflamed and can result in decreased oxygen and nutrient delivery to tissues. In addition, micro vessels are also found to have reduced vessel diameter, vascular density, and diminished blood flow (10, 11). When used in conjunction with HBOT, PEMF therapy may lead to improved microvascular function, blood flow, and therefore tissue and organ health.
News & Research for Inflammatory Bowel Disease:
Adjunctive Hyperbaric Oxygen Therapy promotes successful healing in patients with refractory Crohn’s disease.
To investigate de adjunctive effect of Hyperbaric Oxygen Therapy in a group of patients with refractory Crohn’s disease. A total of 29 subjects with refractory Crohn’s disease were submitted to daily sessions of Hyperbaric Oxygen Therapy, in a 2800 Sechrist Monoplace Hyperbaric Chamber (Sechrist, USA) pressurized to 2.4 ATA. Each session lasted 2 hours. The endpoint was closure of enterocutaneous fistulas and complete healing of Pyoderma Gangrenosum and perineal Crohn’s disease. A total of 829 HBOT sessions were performed and no complications were noted. Overall success rate was 76% (22 cases). Pyoderma Gangrenosum and enterocutaneous fistulas had the highest successful healing rates (100% and 91%, respectively).
Umbilical cord-derived mesenchymal stem cell transplantation combined with hyperbaric oxygen treatment for repair of traumatic brain injury.
Transplantation of umbilical cord-derived mesenchymal stem cells (UC-MSCs) for repair of traumatic brain injury has been used in the clinic. Hyperbaric oxygen (HBO) treatment has long been widely used as an adjunctive therapy for treating traumatic brain injury. UC-MSC transplantation combined with HBO treatment is expected to yield better therapeutic effects on traumatic brain injury. In this study, we established rat models of severe traumatic brain injury by pressurized fluid (2.5-3.0 atm impact force). The injured rats were then administered UC-MSC transplantation via the tail vein in combination with HBO treatment.
Hyperbaric oxygen therapy stimulates colonic stem cells and induces mucosal healing in patients with refractory ulcerative colitis: a prospective case series.
Hyperbaric oxygen (HBO) is used as part of treatment in a variety of clinical conditions. Its use in the treatment of ulcerative colitis has been reported in few clinical reports. We report the effect of HBO on refractory ulcerative colitis exploring one potential mechanism of action. A review of records of patients with refractory ulcerative colitis who received HBO was conducted. Clinical and histopathological scoring was utilised to evaluate the response to HBO therapy (HBOT). All patients manifested clinical improvement by the 40th cycle of HBOT. The median number of stool frequency dropped from seven motions/day (range=3-20) to 1/day (range=0.5-3), which was significant (z=-4.6, p<0.001).
References
- Mattos, Bruno Rafael Ramos de, Maellin Pereira Gracindo Garcia, Julia Bier Nogueira, Lisiery Negrini Paiatto, Cassia Galdino Albuquerque, Caique Lopes Souza, Luís Gustavo Romani Fernandes, Wirla Maria da Silva Cunha Tamashiro, and Patricia Ucelli Simioni. “Inflammatory Bowel Disease: An Overview of Immune Mechanisms and Biological Treatments.” Mediators of Inflammation 2015 (2015). https://doi.org/10.1155/2015/493012.
- Papadakis, K. A., and S. R. Targan. “The Role of Chemokines and Chemokine Receptors in Mucosal Inflammation.” Inflammatory Bowel Diseases 6, no. 4 (November 2000): 303–13. https://doi.org/10.1002/ibd.3780060408.
- Rachmilewitz, D., J. S. Stamler, D. Bachwich, F. Karmeli, Z. Ackerman, and D. K. Podolsky. “Enhanced Colonic Nitric Oxide Generation and Nitric Oxide Synthase Activity in Ulcerative Colitis and Crohn’s Disease.” Gut 36, no. 5 (May 1995): 718–23. https://doi.org/10.1136/gut.36.5.718.
- Akin, M. L., B. M. Gulluoglu, H. Uluutku, C. Erenoglu, E. Elbuken, S. Yildirim, and T. Celenk. “Hyperbaric Oxygen Improves Healing in Experimental Rat Colitis.” Undersea & Hyperbaric Medicine: Journal of the Undersea and Hyperbaric Medical Society, Inc 29, no. 4 (2002): 279–85. https://www.ncbi.nlm.nih.gov/pubmed/12797669
- Granowitz, E. V., E. J. Skulsky, R. M. Benson, J. Wright, J. L. Garb, E. R. Cohen, E. C. Smithline, and R. B. Brown. “Exposure to Increased Pressure or Hyperbaric Oxygen Suppresses Interferon-Gamma Secretion in Whole Blood Cultures of Healthy Humans.” Undersea & Hyperbaric Medicine: Journal of the Undersea and Hyperbaric Medical Society, Inc 29, no. 3 (2002): 216–25. https://www.ncbi.nlm.nih.gov/pubmed/12670123
- Yeh, Ann Ming et al. “Mind-Body Interventions for Pediatric Inflammatory Bowel Disease.” Children (Basel, Switzerland) vol. 4,4 22. 3 Apr. 2017, doi:10.3390/children4040022
- Waśko-Czopnik, Dorota, and Leszek Paradowski. “The influence of deficiencies of essential trace elements and vitamins on the course of Crohn’s disease.” Advances in clinical and experimental medicine : official organ Wroclaw Medical University vol. 21,1 (2012): 5-11.
- Gaby, Alan R. “Intravenous nutrient therapy: the “Myers’ cocktail“. Alternative medicine review: a journal of clinical therapeutic 7 5 (2002): 389-403.
- Yan, Haiyan et al. “Ascorbic acid ameliorates oxidative stress and inflammation in dextran sulfate sodium-induced ulcerative colitis in mice.” International journal of clinical and experimental medicine vol. 8,11 20245-53. 15 Nov. 2015
- Deban, Livija et al. “Multiple pathogenic roles of microvasculature in inflammatory bowel disease: a Jack of all trades” The American journal of pathology vol. 172,6 (2008): 1457-66. doi:10.2353/ajpath.2008.070593
- Hatoum, Ossama A et al. “The vascular contribution in the pathogenesis of inflammatory bowel disease.” American journal of physiology. Heart and circulatory physiology vol. 285,5 (2003): H1791-6. doi:10.1152/ajpheart.00552.2003

