Ulcerative Colitis (UC)
Ulcerative colitis (UC) is an autoimmune inflammatory bowel disease (IBD) characterized by chronic inflammation of the lining of the colon and/or rectum(1). UC is known to involve three main issues: low levels of oxygen in intestinal tissue (hypoxia), increased activity of pro-inflammatory marker T17, and issues with gut flora(2,3,4). These issues result in intestinal sores and ulcers, as well as bloody stool, abdominal pain, fatigue, diarrhea and weight loss (5). Typical treatment starts with 5-aminosalicylic acid, and progresses to corticosteroids, immunomodulators, TNF-inhibitors, and/or colectomy if symptoms persist. These treatments all have adverse side effects, some of which are very severe (5).
Extivita Therapies for Ulcerative Colitis:
Extivita Therapies for Ulcerative Colitis Recovery:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Listen to Bryce’s experience with Hyperbaric Oxygen Therapy to treat Ulcerative Colitis
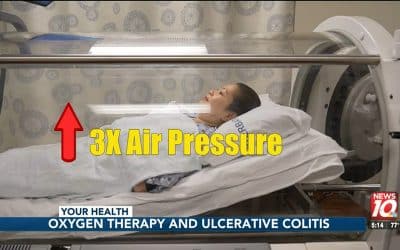
Hyperbaric Oxygen Therapy for Ulcerative Colitis:
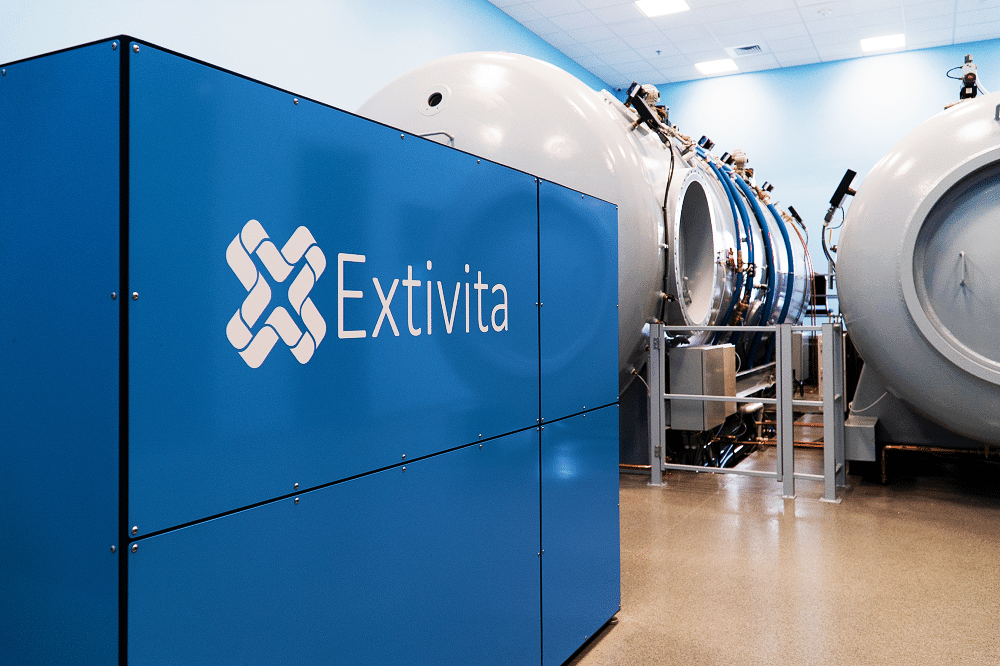
Hyperbaric oxygen therapy (HBOT) may significantly improve ulcerative colitis symptoms with a low risk of adverse side effects(6). HBOT works by increasing tissue oxygen levels (thus combating hypoxia) and is known to reduce inflammation, two main issues implicated in UC patients(7).
Existing studies have found that HBOT is well tolerated by patients with UC and that the positive response rate is roughly 88%(8). HBOT was found to decrease the need for potentially harmful “second-line” therapies such as surgery and biologic therapy in patients whose symptoms were not responding to previous treatment(2). Lastly, HBOT has the potential to heal damaged intestinal tissue by mobilizing stem cells from the bone marrow to the intestines(10).
Effects of HBOT on Ulcerative Colitis:

Decreased Inflammation
Increased Stem Cell Activity
New Blood Vessel Formation
Hyperbaric oxygen therapy stimulates the formation of new blood vessels, healing injured tissues that were unable to get nutrients and oxygen.
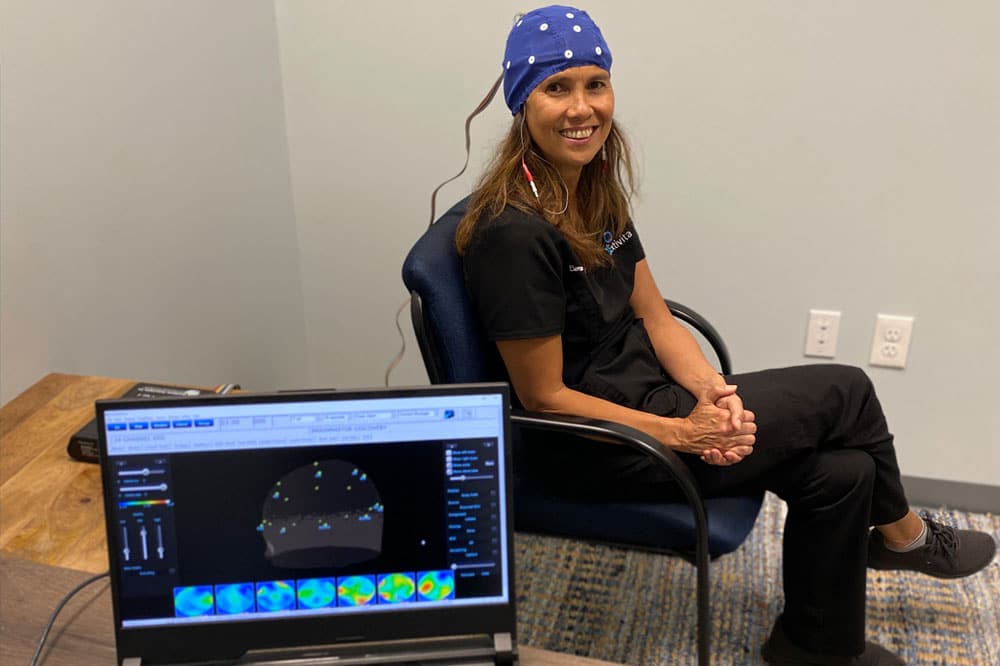
Neurofeedback for Ulcerative Colitis:
Psychological and emotional stressors can trigger inflammatory responses that affect the whole body. In patients with UC, these stressors can cause “flares” resulting in mucosal inflammatory response and UC exacerbations(9). In addition, there has been a significant amount of research showing clear connections between the gut and the brain. Stress, anxiety, and depression can send signals to the gut and vice versa causing brain remodeling and alterations. Neurofeedback can enhance functional connectivity in specific brain regions to reduce the negative effects of psycho/emotional stress responses.
IV Therapy for Ulcerative Colitis:
Research has shown that individuals with IBD have lower circulating levels of total antioxidants in their blood during both the active and asymptomatic stages of disease(11). Inflammation from reactive oxygen and nitrogen species, coupled with depletion of antioxidants, contribute to damage of the intestinal walls in patients with IBD. The Myer’s cocktail provides higher serum levels of antioxidants (compared with oral supplementation) which can decrease inflammation, especially that in IBD. When given with glutathione, the Myer’s cocktail can have a powerful synergistic effect on decreasing inflammation and improving the body’s response to stress.
Main IV Effects:
- Decrease Inflammation
- Increase Stress Response
- Improve Nutrient Deficiencies
- Prevent Tissue Damage


Pulse Electromagnetic Field Therapy for Ulcerative Colitis:
In chronic inflammatory disease like ulcerative colitis, pulse electromagnetic field (PEMF) therapy can be an effective addition to dietary interventions. PEMF therapy helps by correcting imbalances in the immune system, counteracting inflammatory responses, and supporting healing processes(12).
Main Effects of PEMF:
- Improves Circulation
- Increases Delivery of Oxygen and Nutrients to Tissues
- Aids in Removal of Toxins
- Activates Repair Proteins to Help Damaged Tissue
News & Research for Ulcerative Colitis:
Ulcerative Colitis: A New Hope For Healing
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that affects the inner lining of the colon, leading to symptoms such as abdominal pain, diarrhea, fatigue, and rectal bleeding. While conventional treatments like corticosteroids and biologics offer...
Your Health: Oxygen therapy and ulcerative colitis
LANSING, Mich. (WILX) – Hyperbaric oxygen therapy has been around since the 1940′s, when it was first used to treat scuba divers who had decompression sickness. More recently, it’s become a successful treatment to help burn victims and heal wounds. During hyperbaric...
Hyperbaric oxygen therapy could help fight ulcerative colitis, study says
Hyperbaric oxygen therapy has shown promise in treatment for patients with moderate to severe ulcerative colitis, according to a study published in Cellular Molecular Gastroenterology and Hepatology. Hyperbaric oxygen therapy involves breathing pure oxygen in a...
References
- Mattos, Bruno Rafael Ramos de, Maellin Pereira Gracindo Garcia, Julia Bier Nogueira, Lisiery Negrini Paiatto, Cassia Galdino Albuquerque, Caique Lopes Souza, Luís Gustavo Romani Fernandes, Wirla Maria da Silva Cunha Tamashiro, and Patricia Ucelli Simioni. “Inflammatory Bowel Disease: An Overview of Immune Mechanisms and Biological Treatments.” Mediators of Inflammation 2015 (2015). https://doi.org/10.1155/2015/493012.
- Dulai, Parambir S., et al. “Hyperbaric Oxygen Therapy Is Well Tolerated and Effective for Ulcerative Colitis Patients Hospitalized for Moderate-Severe Flares: A Phase 2A Pilot Multi-Center, Randomized, Double-Blind, Sham-Controlled Trial.” The American Journal of Gastroenterology, vol. 113, no. 10, 2018, pp. 1516–23. PubMed, doi:10.1038/s41395-018-0005-z.
- Magalhães, José, et al. “Acute and Severe Hypobaric Hypoxia Increases Oxidative Stress and Impairs Mitochondrial Function in Mouse Skeletal Muscle.” Journal of Applied Physiology (Bethesda, Md.: 1985), vol. 99, no. 4, Oct. 2005, pp. 1247–53. PubMed, doi:10.1152/japplphysiol.01324.2004.
- Semenza, Gregg L. “Oxygen Sensing, Homeostasis, and Disease.” New England Journal of Medicine, vol. 365, no. 6, Massachusetts Medical Society, Aug. 2011, pp. 537–47. Taylor and Francis+NEJM, doi:10.1056/NEJMra1011165.
- “Ulcerative Colitis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 24 Dec 2019, www.mayoclinic.org/diseases-conditions/ulcerative-colitis/diagnosis-treatment/drc-20353331.
- Heyboer, Marvin, et al. “Hyperbaric Oxygen Therapy: Side Effects Defined and Quantified.” Advances in Wound Care, vol. 6, no. 6, June 2017, pp. 210–24. PubMed Central, doi:10.1089/wound.2016.0718.
- Thom, Stephen R. “Hyperbaric Oxygen – Its Mechanisms and Efficacy.” Plastic and Reconstructive Surgery, vol. 127, no. Suppl 1, Jan. 2011, pp. 131S-141S. PubMed Central, doi:10.1097/PRS.0b013e3181fbe2bf.
- Dulai, P. S., et al. “Systematic Review: The Safety and Efficacy of Hyperbaric Oxygen Therapy for Inflammatory Bowel Disease.” Alimentary Pharmacology & Therapeutics, vol. 39, no. 11, 2014, pp. 1266–75. Wiley Online Library, doi:10.1111/apt.12753.
- Mawdsley, Joel E et al. “The effect of acute psychologic stress on systemic and rectal mucosal measures of inflammation in ulcerative colitis.” Gastroenterology vol. 131,2 (2006): 410-9. doi:10.1053/j.gastro.2006.05.017
- Hyperbaric Oxygen Therapy Stimulates Colonic Stem Cells and Induces Mucosal Healing in Patients with Refractory Ulcerative Colitis: A Prospective Case Series – ProQuest. search-proquest-com.go.libproxy.wakehealth.edu, https://search-proquest-com.go.libproxy.wakehealth.edu/docview/2311947674?rfr_id=info%3Axri%2Fsid%3Aprimo. Accessed 7 Aug. 2020.
- Moura, Fabiana Andréa et al. “Antioxidant therapy for treatment of inflammatory bowel disease: Does it work?.” Redox biology vol. 6 (2015): 617-639. doi:10.1016/j.redox.2015.10.006
- Kubat, Nicole J et al. “Effect of pulsed electromagnetic field treatment on programmed resolution of inflammation pathway markers in human cells in culture.” Journal of inflammation research vol. 8 59-69. 23 Feb. 2015, doi:10.2147/JIR.S78631