Osteoarthritis
Osteoarthritis (OA) is estimated to affect roughly 27 million Americans, with those older than 60 having the highest incidence (1). The main symptoms are swelling, pain, stiffness, and possible grinding at the affected joint. Most OA treatments focus on relieving joint pain and optimize function to improve quality of life (2).
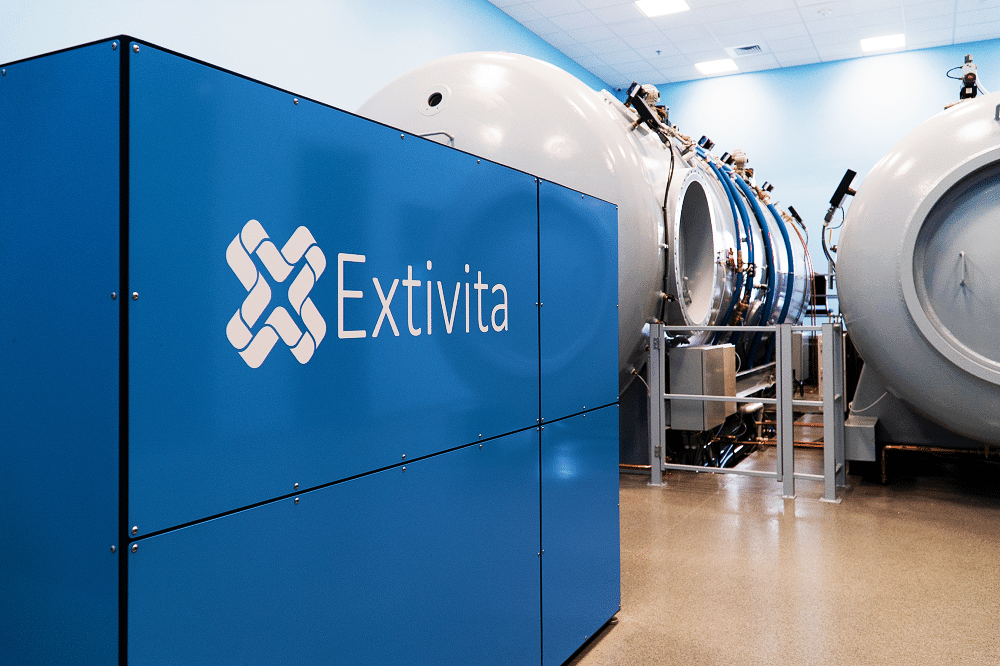
Extivita Therapies for Osteoarthritis:
Extivita Therapies Osteoarthritis Recovery:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Hyperbaric Oxygen Therapy for Osteoarthritis:
Additionally, research on rheumatoid arthritis, which presents with inflammation and pain symptoms like OA, showed decreased feelings of pain in a human study (5). Beyond treating symptoms of OA, recent research suggests that HBOT may stimulate the production of new cartilage at joints (6).
Effects of HBOT on Osteoarthritis:

Decreased Inflammation
Increased Stem Cell Activity

Neurofeedback for Osteoarthritis:
There is some evidence to suggest that neurofeedback may improve dynamic stability for those with osteoarthritis following knee replacement. Neurofeedback may work by strengthening the connections between the brain and the limbs and may be an appropriate supplementary therapy to traditional physical rehabilitation (6).
IV Therapy for Osteoarthritis:
Research has shown that the imbalance between free radical burden and free radical scavenging mechanisms is a significant part of OA disease development (7). Increased free radical burden has been shown to cause inflammation, fibrosis, and pain in local tissues between joint compartments. This can lead to cartilage destruction, joint changes from inflammation, and subsequent transition to apparent OA. Vitamin C is a potent antioxidant that protects cells from damage caused be free radicals (8). Myers’ cocktail and IV glutathione can provide oxidative stress resistance (9-10).


Pulsed Electromagnetic Field Therapy for Osteoarthritis:
Osteoarthritis is a degenerative disease which causes joint pain and ultimately loss of joint function and disablement. PEMF’s effect on improving microcirculation/blood flow has been shown to reduce inflammation, improve mobility and alleviate pain(11-12). In fact, a review of 16 studies found that PEMF effectively reduces pain and stiffness while improving physical function in people with osteoarthritis(13).
News & Research for Osteoarthritis:
Case report: intestinal pneumatosis
To present a recent to increase understanding, diagnosis and treatment of intestinal pneumatosis clinical case, considering the distinctive characteristics of the disease and to expand knowledge about the management of this condition. The case of a female patient aged 65, originally from Bolivia, with a history of osteoarthritis, osteoporosis, asthma and allergies repetition occurs. The patient was admitted to the Department of Surgery No. 1 HNC in November 2015, with an unclear clinical picture. During admission of air bubbles present in the colonic mucosa and tumor lesion is discovered duodenum. Quickly it begins with treatment and adequate support for stabilization. A literature search and an update of the latest updates regarding this disease arises. medical seekers popularity as PUBMED, UP TO DATE, VBS were used. a series of articles about it were selected.
Hyperbaric oxygen protects mandibular condylar chondrocytes from interleukin-1β-induced apoptosis via the PI3K/AKT signaling pathway
Objectives: Mandibular condylar chondrocyte apoptosis is mainly responsible for the development and progression of temporomandibular joint osteoarthritis (TMJ-OA). Interleukin-1β (IL-1β) generally serves an agent that induces chondrocyte apoptosis. Hyperbaric oxygen (HBO) treatment increases proteoglycan synthesis in vivo. We explore the protective effect of HBO on IL-1β-induced mandibular condylar chondrocyte apoptosis in rats and the potential molecular mechanisms. Methods: Chondrocytes were isolated from the TMJ of 3-4-week old Sprague-Dawley rats. The Cell Counting Kit-8 (CCK-8) assay was used to determine cell viability. The phosphorylated phosphoinositide-3 kinase (p-PI3K), phosphorylated AKT (p-Akt), type II collagen (COL2), and aggrecan (AGG) content was detected by immunofluorescence, immunocytochemistry and western blotting. The expression of Pi3k, Akt, Col2 and Agg mRNA was measured using real-time quantitative polymerase chain reaction (RT-qPCR). Results: HBO inhibited the cytotoxicity and apoptosis induced by IL-1β (10 ng/mL) in the mandibular condylar chondrocytes. HBO also decreased the IL-1β activity that decreased p-PI3K and p-AKT levels, and increased COL2 and AGG expression, with the net effect of suppressing extracellular matrix degradation. Conclusions: These data suggest that HBO may protect mandibular condylar chondrocytes against IL-1β-induced apoptosis via the PI3K/AKT signaling pathway, and that it may promote the expression of mandibular condylar chondrocyte extracellular matrix through the PI3K/AKT signaling pathway.
Rehabilitation of the patients with osteoarthritis.
Under the term “osteoarthritis” (OA) is currently meant a clinical syndrome resulting from the combined effect of articular pain and disordered functional activity leading to the deterioration of the quality of life of the patients. The principal objective of rehabilitation of the patients presenting with GA in which all patients with this condition are in need practically after each next aggravation of the pathological process is to relive pain syndrome and restore the functional ability of the joints lost or deteriorated after each exacerbation in order to eventually improve the quality of life of the patients experiencing the constantly progressing degenerative process in the musculoskeletal system.
References
- “The Basics of Osteoarthritis.” WebMD. Accessed July 18, 2019. https://www.webmd.com/osteoarthritis/guide/osteoarthritis-basics.
- “Diseases and Conditions Osteoarthritis.” American College of Rheumatology, March 2019. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Osteoarthritis.
- Sellam, Jérémie, and Francis Berenbaum. “The Role of Synovitis in Pathophysiology and Clinical Symptoms of Osteoarthritis.” Nature Reviews Rheumatology 6, no. 11 (November 2010): 625–35. https://doi.org/10.1038/nrrheum.2010.159.
- Thom, Stephen R. “Hyperbaric Oxygen – Its Mechanisms and Efficacy.” Plastic and Reconstructive Surgery 127, no. Suppl 1 (January 2011): 131S-141S. https://doi.org/10.1097/PRS.0b013e3181fbe2bf.
- Slade, John B., Mary V. Potts, Alan M. Flower, Karen M. Sky, Michelle T. Sit, and Thomas W. Schmidt. “Pain Improvement in Rheumatoid Arthritis with Hyperbaric Oxygen: Report of Three Cases.” Undersea & Hyperbaric Medicine: Journal of the Undersea and Hyperbaric Medical Society, Inc 43, no. 4 (August 2016): 467–72. https://www.ncbi.nlm.nih.gov/pubmed/28763177
- Chen, Hang, Gaoyi Wu, Qi Sun, Yabing Dong, and Huaqiang Zhao. “Hyperbaric Oxygen Protects Mandibular Condylar Chondrocytes from Interleukin-1β-Induced Apoptosis via the PI3K/AKT Signaling Pathway.” American Journal of Translational Research 8, no. 11 (November 15, 2016): 5108–17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5126354/
- Jamebozorgi, Ali asghar, et al. “The Effect of Neurofeedback on Postural Balance and Attention in Patients Suffering From Knee Osteoarthritis With Bilateral Total Knee Replacement: A Pilot Study.” Archives of Rehabilitation, vol. 21, no. 1, Archives of Rehabilitation, Mar. 2020, pp. 4–4.
- McAlindon, Timothy E., Paul Jacques, Yuqing Zhang, Marian T. Hannan, Piran Aliabadi, Barbara Weissman, David Rush, Daniel Levy, and David T. Felson. “Do Antioxidant Micronutrients Protect against the Development and Progression of Knee Osteoarthritis?” Arthritis & Rheumatism 39, no. 4 (1996): 648–56. https://doi.org/10.1002/art.1780390417.
- Ziskoven, Christoph et al. “Oxidative stress in secondary osteoarthritis: from cartilage destruction to clinical presentation?.” Orthopedic reviews vol. 2,2 (2010): e23. doi:10.4081/or.2010.e23
- Shouan Zhu, Dawid Makosa, Benjamin Miller & Timothy M. Griffin (2020) Glutathione as a mediator of cartilage oxidative stress resistance and resilience during aging and osteoarthritis, Connective Tissue Research, 61:1, 34-47, DOI: 10.1080/03008207.2019.1665035
- Kaitlin S, Sheena S, Magda H. Pilot Study: Pulsed Electromagnetic Field Therapy (PEMFT) Alleviates Symptoms of Osteoarthritis. Nov Tech Arthritis Bone Res. 2017; 1(5) : 555571.
- Gutterman, David D et al. “The Human Microcirculation: Regulation of Flow and Beyond.” Circulation research vol. 118,1 (2016): 157-72. doi:10.1161/CIRCRESAHA.115.305364
- Yang, Xiaotian, et al. “Effects of Pulsed Electromagnetic Field Therapy on Pain, Stiffness, Physical Function, and Quality of Life in Patients With Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Placebo-Controlled Trials.” Physical Therapy, vol. 100, no. 7, July 2020, pp. 1118–31. PubMed,.



