Concussion, PCS, & mTBI
The importance of proper healing from Mild Traumatic Brain Injuries (mTBIs), such as concussions, has been historically undervalued(1). Thankfully, recent years have brought an increased focus towards mTBIs in the United States, especially towards their potential long-term consequences(2).
Acute symptoms such as slow response time, irritability, and low energy may resolve on their own, but sometimes they can persist and evolve into long-lasting cognitive, behavioral, and communicative disabilities(2). When these symptoms remain present 3 months post-injury, the individual is considered to have “Post-Concussion Syndrome” or “PCS”(3).
We strongly recommend Hyperbaric Oxygen Therapy (HBOT) as a primary treatment for mTBIs and PCS. We also recommend Neurofeedback Therapy, IV Therapy, and Pulsed-Electromagnetic Field Therapy (PEMF) as supporting therapies to maximize your healing.
Extivita Therapies for Concussion, PCS, & mTBI:
EXTIVITA THERAPIES FOR CONCUSSION, PCS, & mTBI RECOVERY:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Listen to John’s experience with Hyperbaric Oxygen Therapy to treat his Concussion & Post Concussion Syndrome
Hyperbaric Oxygen Therapy for Concussion:
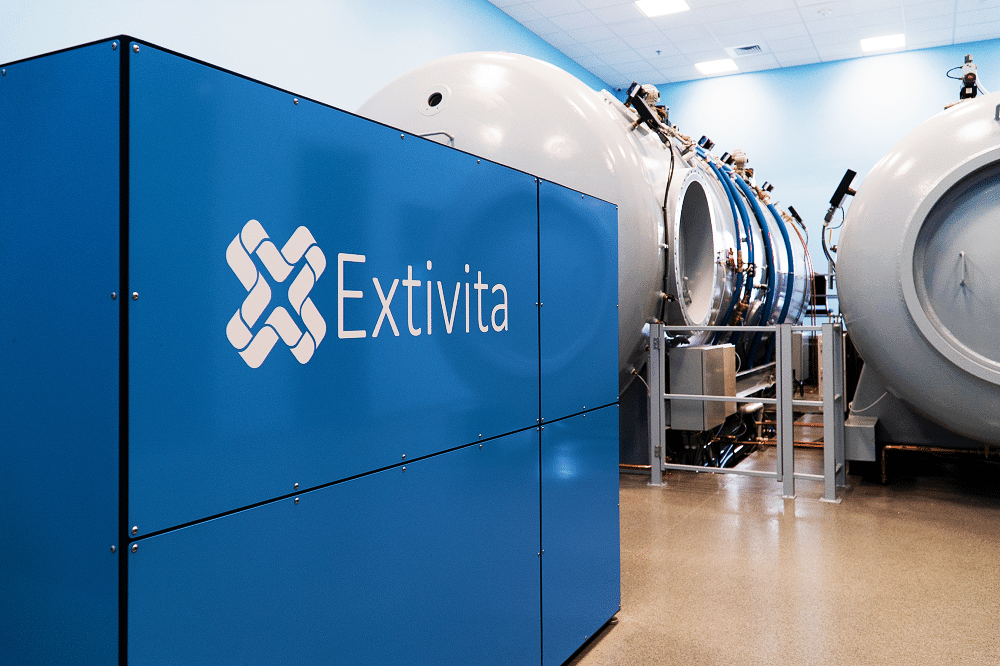
HBOT has repeatedly been shown to improve many PCS symptoms, even years after initial injury(4-7). Specific categories of improvement include memory, depression, anxiety, post-traumatic stress disorder (PTSD) ratings, sleep quality, and overall quality of life(4-6). These positive findings are typically achieved after completing 40 HBOT treatments, most commonly at a pressure of 1.5-2.0 atmospheres(4-6).
Research suggests that these improvements are due to improved tissue oxygenation, cellular metabolism, and mitochondrial function as well as a well-regulated inflammatory response. These effects are a direct result of HBOT(8). Lastly, the benefits of HBOT for mTBI are likely most significant when administered soon after initial injury, although studies have found that improvements can still occur up to 5 years post-mTBI(7).
Effects of HBOT on Concussion, PCS, & mTBI:
New Blood Vessel Formation
Increased Stem Cell Activity

Decreased Inflammation

Neurofeedback for Concussion:
Neurofeedback may be a beneficial adjunctive therapy for those experiencing mTBI or PCS symptoms. After a mTBI, the brain must form new neural pathways to account for any brain tissue damaged by the mTBI. These new connections play a vital role in restoring healthy brain function, and neurofeedback has been shown to help establish and strengthen such connections(9). While there are few studies on neurofeedback and mTBIs specifically, existing research has found improvements in attention in people with mTBI following neurofeedback therapy(10).
IV Therapy for Concussion:
Both our Myer’s cocktail IV and NAD+ Trio IV can help mTBI recovery. After mTBIs occur, the brain typically shows higher levels of inflammation and oxidative stress, both of which contribute to brain cell damage and persistent mTBI symptoms(11-12).
Replenishing the brain with Vitamin C, a component of the Myer’s IV cocktail, decreases this inflammation and oxidative stress, slows down cell damage, neutralizes toxins, and reduces brain swelling(13). Vitamin B12, which is also in the Myer’s cocktail, has been reported to promote nerve repair after TBI as well(14). The combined benefits of vitamin C and B12 on the brain can help minimize brain cell damage and improve cognitive function.
We also recommend our NAD+ Trio IV for mTBI due to NAD+’s role in energy production, mitochondrial function, and DNA repair. Following a mTBI, NAD+ levels become depleted, cellular detoxification is impaired, and mitochondria do not function as well(15-16). This can result in a cascade of damaging effects that leads to neurodegeneration (brain cell death). Our NAD+ Trio IV replenishes your NAD+ levels, helping restore mitochondrial function and reduce the severity and resulting damage of such a cascade(15).


Pulsed Electromagnetic Field Therapy for Concussion:
Research has shown that pulsed electromagnetic field (PEMF) therapy supports the brain in numerous ways, some of which include improving cognitive function, reducing stress, and relieving headaches(17). Specific to mTBIs, PEMF has been shown to decrease neuroinflammation, reduce cytokine levels (such as IL-1B)(18), reduce phobias, and significantly improve psychological depression following mTBI(17-18).
News & Research for Concussion:
Baseline vestibular and auditory findings in a trial of post-concussive syndrome
Abstract: Previous studies have reported high rates of auditory and vestibular-balance deficits immediately following head injury. This study uses a comprehensive battery of assessments to characterize auditory and vestibular function in 71 U.S. military service...
Review of recent non-hyperbaric oxygen interventions for mild traumatic brain injury.
Traumatic brain injury (TBI) affects 3.2 to 5.3 million persons in the United States (U.S.), and the impact in the U.S. military is proportionally higher. Consensus is lacking regarding an accepted outcome to measure the effectiveness of interventions to improve the symptoms associated with TBI, and no standard-of-care treatment exists for mild TBI (mTBI). A recent literature review evaluated hyperbaric oxygen therapy (HBO₂) interventions, and findings were mixed. We conducted a systematic review of non-HBO₂ mTBI interventional trials published in 2005-2015 in military and civilian populations. A total of 154 abstracts, seven randomized controlled trials (RCTs) and five pilot studies were reviewed. RCTs were evaluated using Consolidated Standards of Reporting Trials criteria. Results indicated that studies published within the period of review were small pilot studies for rehabilitation therapy and motion capture or virtual reality gaming interventions. Neuropsychological assessments were commonly specified outcomes, and most studies included a combination of symptom and neuropsychological assessments. Findings indicated a lack of large-scale, well-controlled trials to address the symptoms and sequelae of this condition, but results of small exploratory studies show evidence of potentially promising interventions.
Executive summary: The Brain Injury and Mechanism of Action of Hyperbaric Oxygen for Persistent Post-Concussive Symptoms after Mild Traumatic Brain Injury (mTBI) (BIMA) Study.
The Brain Injury and Mechanism of Action of Hyperbaric Oxygen for Persistent Post-Concussive Symptoms after Mild Traumatic Brain Injury (mTBI) (BIMA) study, sponsored by the Department of Defense and held under an investigational new drug application by the Office of the Army Surgeon General, is one of the largest and most complex clinical trials of hyperbaric oxygen (HBO₂) for post-concussive symptoms (PCS) in U.S. military service members.
References
- Mann, Aneetinder, et al. “Concussion Diagnosis and Management: Knowledge and Attitudes of Family Medicine Residents.” Canadian Family Physician, vol. 63, no. 6, The College of Family Physicians of Canada, June 2017, pp. 460–66.
- Silverberg, Noah D., et al. “Management of Concussion and Mild Traumatic Brain Injury: A Synthesis of Practice Guidelines.” Archives of Physical Medicine and Rehabilitation, vol. 101, no. 2, Feb. 2020, pp. 382–93. ScienceDirect, doi:10.1016/j.apmr.2019.10.179.
- Ryan, Laurie M., and Deborah L. Warden. “Post Concussion Syndrome.” International Review of Psychiatry (Abingdon, England), vol. 15, no. 4, Nov. 2003, pp. 310–16. PubMed, doi:10.1080/09540260310001606692.
- Harch, Paul G., et al. “Hyperbaric Oxygen Therapy for Mild Traumatic Brain Injury Persistent Postconcussion Syndrome: A Randomized Controlled Trial.” Medical Gas Research, vol. 10, no. 1, Mar. 2020, pp. 8–20. PubMed, doi:10.4103/2045-9912.279978.
- Mozayeni, B. Robert, et al. “The National Brain Injury Rescue and Rehabilitation Study – a Multicenter Observational Study of Hyperbaric Oxygen for Mild Traumatic Brain Injury with Post-Concussive Symptoms.” Medical Gas Research, vol. 9, no. 1, Mar. 2019, pp. 1–12. PubMed, doi:10.4103/2045-9912.254636.
- Weaver, Lindell K., et al. “Hyperbaric Oxygen for Post-Concussive Symptoms in United States Military Service Members: A Randomized Clinical Trial.” Undersea & Hyperbaric Medicine: Journal of the Undersea and Hyperbaric Medical Society, Inc, vol. 45, no. 2, Apr. 2018, pp. 129–56.
- Boussi-Gross, Rahav, et al. “Hyperbaric Oxygen Therapy Can Improve Post Concussion Syndrome Years after Mild Traumatic Brain Injury – Randomized Prospective Trial.” PLoS ONE, vol. 8, no. 11, Nov. 2013. PubMed Central, doi:10.1371/journal.pone.0079995.
- Efrati, Shai, and Eshel Ben-Jacob. “Reflections on the Neurotherapeutic Effects of Hyperbaric Oxygen.” Expert Review of Neurotherapeutics, vol. 14, no. 3, Mar. 2014, pp. 233–36. PubMed, doi:10.1586/14737175.2014.884928.
- Munivenkatappa, Ashok, et al. “EEG Neurofeedback Therapy: Can It Attenuate Brain Changes in TBI?” NeuroRehabilitation, vol. 35, no. 3, IOS Press, Jan. 2014, pp. 481–84. content.iospress.com, doi:10.3233/NRE-141140.
- Hershaw, Jamie, et al. “Changes in Attentional Processing Following Neurofeedback in Patients with Persistent Post-Concussive Symptoms: A Pilot Study.” Brain Injury, vol. 34, no. 13–14, Taylor & Francis, Dec. 2020, pp. 1723–31. Taylor and Francis+NEJM, doi:10.1080/02699052.2020.1812720.
- Chaban, Viktoriia, et al. “Systemic Inflammation Persists the First Year after Mild Traumatic Brain Injury: Results from the Prospective Trondheim Mild Traumatic Brain Injury Study.” Journal of Neurotrauma, vol. 37, no. 19, Mary Ann Liebert, Inc., publishers, Oct. 2020, pp. 2120–30. liebertpub.com (Atypon), doi:10.1089/neu.2019.6963.
- Toklu, Hale Zerrin, and Nihal Tümer. “Oxidative Stress, Brain Edema, Blood–Brain Barrier Permeability, and Autonomic Dysfunction from Traumatic Brain Injury.” Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects, edited by Firas H. Kobeissy, CRC Press/Taylor & Francis, 2015. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK299195/.
- Leichtle, Stefan W et al. “High-Dose Intravenous Ascorbic Acid: Ready for Prime Time in Traumatic Brain Injury?.” Neurocritical care vol. 32,1 (2020): 333-339. doi:10.1007/s12028-019-00829-x
- Wu, Fangfang et al. “Vitamin B12 Enhances Nerve Repair and Improves Functional Recovery After Traumatic Brain Injury by Inhibiting ER Stress-Induced Neuron Injury.” Frontiers in pharmacology vol. 10 406. 24 Apr. 2019, doi:10.3389/fphar.2019.00406
- Won, Seok Joon et al. “Prevention of traumatic brain injury-induced neuron death by intranasal delivery of nicotinamide adenine dinucleotide.” Journal of neurotrauma vol. 29,7 (2012): 1401-9. doi:10.1089/neu.2011.2228
- Klimova, Nina, Adam Fearnow, and Tibor Kristian. “Role of NAD+—Modulated Mitochondrial Free Radical Generation in Mechanisms of Acute Brain Injury.” Brain Sciences 10.7 (2020): 449. Crossref. Web
- Pawluk, William. “The role of pulsed magnetic fields in the management of concussion and traumatic brain injury.” The Journal of Science and Medicine vol. 1, 2 (2019)
- Rasouli, Jonathan et al. “Attenuation of interleukin-1beta by pulsed electromagnetic fields after traumatic brain injury.” Neuroscience letters vol. 519,1 (2012): 4-8. doi:10.1016/j.neulet.2012.03.089
