Spinal Cord Injuries
An estimated 291,000 persons live with a spinal cord injury (SCI), with roughly 17,730 new cases occurring each year(1). Current research and treatments focus on reducing the “secondary injury cascade” that begins immediately after the initial spinal cord trauma(2). This cascade occurs during either the sub-acute (weeks to months after initial injury) or chronic phase (months to years after initial injury), or during both (3). The severity of this secondary damage directly impacts further bodily damage and the restorative process.
Fortunately, research has shown a correlation between reduced secondary damage and improved neurological outcomes(4, 5). Therapies that can reduce the severity of the secondary injury cascade, such as hyperbaric oxygen therapy, have the potential to reduce the cellular damage that occurs post-injury, and therefore improve neurological outcomes.
Extivita Therapies for Spinal Cord Injuries:
Extivita Therapies Spinal Cord Injury Recovery:
Hyperbaric Oxygen Therapy

Neurofeedback
Supplements

Nutritional IV Therapy
Pulsed Electromagnetic Field Therapy
Ryley’s experience with
Hyperbaric Oxygen Therapy
to treat his
Spinal Cord Injury
Hyperbaric Oxygen Therapy for Spinal Cord Injury:
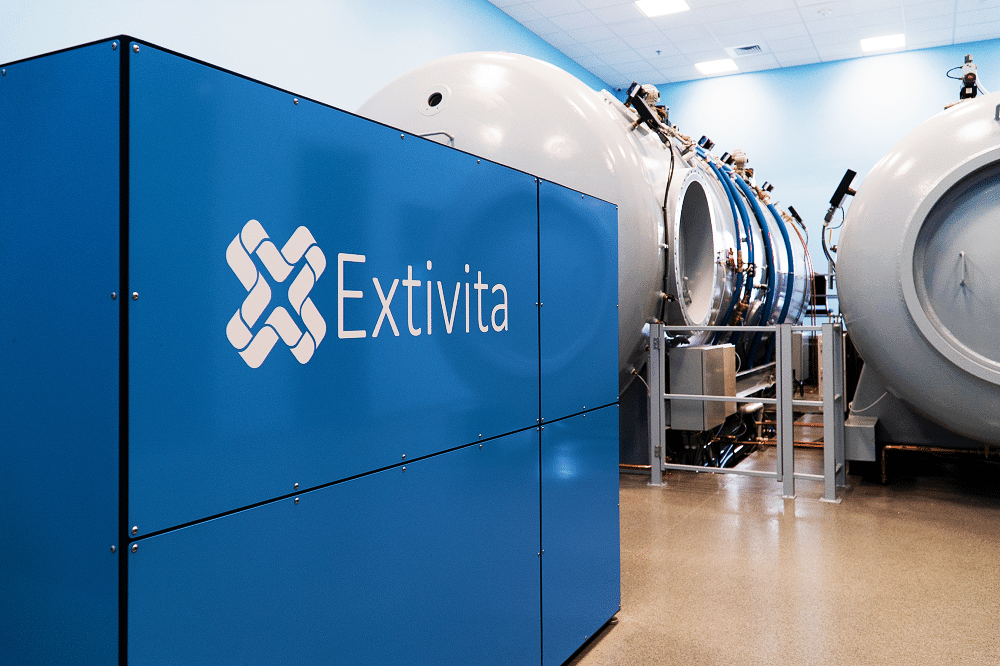
Hyperbaric Oxygen Therapy (HBOT) increases oxygen to the damaged spinal cord tissue, thereby decreasing the cell death and damage that can occur for weeks to months after initial injury (6, 7). Additionally, HBOT decreases spinal cord edema (swelling) and inflammation(3) and has been shown to reduce synaptic and dendritic degeneration in animal models(8).
Synaptic and dendritic degeneration refers to the degradation of connections between nerve cells, which are essential for healthy neurological function. Reducing such degeneration via HBOT may preserve connections in the spinal cord and brain and thus decrease the severity of neurological impairment.
HBOT Research Shows Improvement To:
- Reduces cell death
- Reduces inflammation and swelling
- Reduces oxidative stress
Effects of HBOT on Spinal Cord Injury:

Decreased Inflammation
New Blood Vessel Formation
Increased Stem Cell Activity

Neurofeedback for Spinal Cord Injury:
Neurofeedback may help relieve the central neuropathic pain (CNP) that 50% of SCI patients experience(9-10). CNP is characterized by burning, aching, and prickling sensations that often lead to anxiety and sleep issues, as well as a lower quality of life(9, 11-12). There is some evidence that neurofeedback therapy can reduce ratings of pain in SCI patients with CNP. One study found that 80% of study participants experienced statistically significant pain reduction following sessions of alpha reward training(10). Given this, we recommend neurofeedback therapy for people with SCI who may not be responding to traditional CNP treatment, and for those looking for an alternative method of pain relief.
IV Therapy for Spinal Cord Injury:
Nutritional IV therapy has strong potential to limit that damage of the secondary injury cascade that occurs post-SCI. A hallmark of the secondary phase of SCI is oxidative stress, which occurs when levels of reactive oxygen and/or nitrogen species are elevated(13-14). Brain cells are particularly susceptible to damage from oxidative stress, but such damage can be reduced by improving antioxidant defenses(15).
We recommend our NAD+ IV trio for people with SCI. This trio includes NAD+, a Myer’s Cocktail IV, and a glutathione IV. Both the Myer’s Cocktail IV and glutathione IV have powerful antioxidant effects that may reduce the secondary injury cascade by combating oxidative stress(16-17). The NAD+ can also provide benefits for SCI by improving mitochondrial function, which is impaired in those with SCI(13, 18).


Pulsed Electromagnetic Field Therapy for Spinal Cord Injury:
There is some evidence to suggest that pulsed electromagnetic field (PEMF) therapy may promote functional recovery and reduce the secondary injury cascade in those with SCI. These benefits are likely due to PEMF’s ability to reduce inflammation and oxidative stress, both of which are involved in the secondary injury phase of SCI(19).
News & Research for Spinal Cord Injury:
Hyperbaric Oxygen Therapy after Acute Thoracic Spinal Cord Injury: Improvement of Locomotor Recovery in Rats.
The aim of this study was to analyze the effectiveness of hyperbaric therapy (HT) using mild and moderate models of spinal cord injury (SCI). SCI can cause permanent impairment with socioeconomic consequences. The motor deficit occurs by two mechanisms: destruction of neuronal cells and local inflammatory response, resulting in hypoxia. HT acts by increasing oxygen in the injured area. Thoracic laminectomy was performed in 72 female Wistar rats. The MASCIS impactor was used at 12.5 mm (n = 35) and 25 mm (n = 35) of height to perform, respectively, mild and moderate SCI. Muscle strength was assessed through the Basso, Beattie, and Bresnahan scale (BBB) on days 1, 7, 14, 21, and 28 after SCI. The animals were randomized into five subgroups with seven animals each: (1) control group had SCI without HT; (2) HT 30 minutes after SCI; (3) HT 30 minutes after SCI and daily for 7 days; (4) HT 12 hours after SCI; and (5) HT 12 hours after SCI and daily for 7 days. HT was performed at 2.5 atm for 1 hour.
Decompression sickness among diving fishermen in Mexico: observational retrospective analysis of DCS in three sea cucumber fishing seasons.
The probabilities of decompression sickness (DCS) among diving fishermen are higher than in any other group of divers. Diving behavior of artisanal fishermen has been directed mainly to target high-value species. The aim of this study was to learn about the occurrence of DCS derived from sea cucumber harvesting in the Yucatán Peninsula, Mexico. We conducted a retrospective chart review of diving fishermen treated at a multiplace hyperbaric chamber in Tizimín, Mexico. In total, 233 recompression therapies were rendered to 166 diving fishermen from 2014 to 2016. The average age was 36.7 ± 9.2 years (range: 20-59 years); 84.3% had experienced at least one DCS event previously. There was a correlation between age and DCS incidents (F: 8.3; R2: 0.07) and differences in the fishing depth between seasons (H: 9.99; p⟨0.05). Musculoskeletal pain was the most frequently reported symptom. Three divers, respectively, suffered permanent hearing loss, spinal cord injury and fatal outcome. Diving fishermen experience DCS at an alarmingly high rate, probably due to the type of species targeted, given the requirements in each case. Understanding divers’ behaviors and their incentives while in pursuit of high-value species such as sea cucumber could help to find ways to mitigate health risks and help enforce regulation.
Relationship between clinical and radiologic findings of spinal cord injury in decompression sickness.
Decompression sickness may involve the central nervous system. The most common site is spinal cord. This study was conducted to determine the relationship between magnetic resonance(MR) imaging findings of spinal damage. We conducted a retrospective review of 12 patients (male=10, female=2) who presented with spinal cord symptoms. We investigated their clinical features, neurological findings and radiologic findings. The depth and bottom time of the dive were 34.5 meters (range 22-56) and 22.7 minutes (range 10-55) respectively. Most divers ascended within appropriate time frame as shown by the decompression tables. The most frequent initial symptoms were lower limb weakness (n=12), followed by sensory disturbances (n=10) and bladder dysfuction (n=5). The chief radiologic abnormalities were continuous (n=3), or non-continuous (n=5) high-signal intensity on T2-weighted images at posterior paramedian portion of the spinal cord, mainly thoracic level. There were no abnormal findings in the remaining four (4) patients, and they showed good prognosis. All patients were treated with hyperbaric oxygen therapy and some received high-dose dexamethasone. On discharge, five (5) patients had made a full recovery, seven (7) had some residual neurological sequelae, and all patients except one (1) regained normal bladder function. Spinal cord decompression sickness is a neurological emergency. Early recognition and treatment may minimize neurological damage. Initial normal finding in MR imaging was a good predictor for prognosis in spinal decompression sickness.
References
- “Home Page – NSCISC Application.” Accessed June 19, 2019. https://www.nscisc.uab.edu/.
- “Spinal Cord Injury Information: Levels, Causes, Recovery.” Accessed June 19, 2019. https://www.shepherd.org/patient-programs/spinal-cord-injury/about#FAQ3.
- Oyinbo, Charles Aidemise. “Secondary Injury Mechanisms in Traumatic Spinal Cord Injury: A Nugget of This Multiply Cascade.” Acta Neurobiologiae Experimentalis 71, no. 2 (2011): 281–99. https://pdfs.semanticscholar.org/8131/2216495186e1d35f6958c59587714efca557.pdf
- Dumont, R. J., D. O. Okonkwo, S. Verma, R. J. Hurlbert, P. T. Boulos, D. B. Ellegala, and A. S. Dumont. “Acute Spinal Cord Injury, Part I: Pathophysiologic Mechanisms.” Clinical Neuropharmacology 24, no. 5 (October 2001): 254–64. https://www.ncbi.nlm.nih.gov/pubmed/11586110
- Kwon, Brian K., Wolfram Tetzlaff, Jonathan N. Grauer, John Beiner, and Alexander R. Vaccaro. “Pathophysiology and Pharmacologic Treatment of Acute Spinal Cord Injury.” The Spine Journal 4, no. 4 (July 1, 2004): 451–64. https://doi.org/10.1016/j.spinee.2003.07.007
- Kelly, D. L., K. R. Lassiter, A. Vongsvivut, and J. M. Smith. “Effects of Hyperbaric Oxygenation and Tissue Oxygen Studies in Experimental Paraplegia.” Journal of Neurosurgery 36, no. 4 (April 1972): 425–29. https://doi.org/10.3171/jns.1972.36.4.0425.
- Emery, E., P. Aldana, M. B. Bunge, W. Puckett, A. Srinivasan, R. W. Keane, J. Bethea, and A. D. Levi. “Apoptosis after Traumatic Human Spinal Cord Injury.” Journal of Neurosurgery 89, no. 6 (December 1998): 911–20. https://doi.org/10.3171/jns.1998.89.6.0911.
- Ying, Xinwang, Wenzhan Tu, Sisi Li, Qiaoyun Wu, Xiaolong Chen, Ye Zhou, Jie Hu, Guanhu Yang, and Songhe Jiang. “Hyperbaric Oxygen Therapy Reduces Apoptosis and Dendritic/Synaptic Degeneration via the BDNF/TrkB Signaling Pathways in SCI Rats.” Life Sciences 229 (July 15, 2019): 187–99. https://doi.org/10.1016/j.lfs.2019.05.029.
- Siddall, Philip J., et al. “A Longitudinal Study of the Prevalence and Characteristics of Pain in the First 5 Years Following Spinal Cord Injury.” Pain, vol. 103, no. 3, June 2003, pp. 249–57. ScienceDirect, doi:10.1016/S0304-3959(02)00452-9.
- Vučković, Aleksandra, et al. “EEG Correlates of Self-Managed Neurofeedback Treatment of Central Neuropathic Pain in Chronic Spinal Cord Injury.” Frontiers in Neuroscience, vol. 13, Frontiers, 2019. Frontiers, doi:10.3389/fnins.2019.00762.
- Finnerup, Nanna B., et al. “Neuropathic Pain Clinical Trials: Factors Associated with Decreases in Estimated Drug Efficacy.” Pain, vol. 159, no. 11, Nov. 2018, pp. 2339–46. PubMed Central, doi:10.1097/j.pain.0000000000001340.
- Middleton, James, et al. “Relationship Between Quality of Life and Self-Efficacy in Persons With Spinal Cord Injuries.” Archives of Physical Medicine and Rehabilitation, vol. 88, no. 12, Dec. 2007, pp. 1643–48. ScienceDirect, doi:10.1016/j.apmr.2007.09.001.
- Azbill, Robert D., et al. “Impaired Mitochondrial Function, Oxidative Stress and Altered Antioxidant Enzyme Activities Following Traumatic Spinal Cord Injury.” Brain Research, vol. 765, no. 2, Aug. 1997, pp. 283–90. ScienceDirect, doi:10.1016/S0006-8993(97)00573-8.
- Pizzino, Gabriele, et al. “Oxidative Stress: Harms and Benefits for Human Health.” Oxidative Medicine and Cellular Longevity, vol. 2017, 2017. PubMed Central, doi:10.1155/2017/8416763.
- Jia, Z., et al. “Oxidative Stress in Spinal Cord Injury and Antioxidant-Based Intervention.” Spinal Cord, vol. 50, no. 4, 4, Nature Publishing Group, Apr. 2012, pp. 264–74. www.nature.com, doi:10.1038/sc.2011.111.
- Carr, Anitra C., and Silvia Maggini. “Vitamin C and Immune Function.” Nutrients, vol. 9, no. 11, Nov. 2017. PubMed Central, doi:10.3390/nu9111211.
- Forman, Henry Jay, et al. “Glutathione: Overview of Its Protective Roles, Measurement, and Biosynthesis.” Molecular Aspects of Medicine, vol. 30, no. 1–2, Apr. 2009, pp. 1–12. PubMed, doi:10.1016/j.mam.2008.08.006.
- Johnson, Sean, and Shin-ichiro Imai. “NAD + Biosynthesis, Aging, and Disease.” F1000Research, vol. 7, Feb. 2018. PubMed Central, doi:10.12688/f1000research.12120.1.
- Wang, Chunyan, et al. “Lowfrequency Pulsed Electromagnetic Field Promotes Functional Recovery, Reduces Inflammation and Oxidative Stress, and Enhances HSP70 Expression Following Spinal Cord Injury.” Molecular Medicine Reports, vol. 19, no. 3, Spandidos Publications, Mar. 2019, pp. 1687–93. www.spandidos-publications.com, doi:10.3892/mmr.2019.9820.
