Neurofeedback
Neurofeedback is training for your brain, just like the gym is training for your muscles. However, instead of training to grow bigger muscles, neurofeedback trains your brain to work harmoniously and efficiently towards a more desired, healthy state.
Why Neurofeedback?
Neurofeedback training can be vital for those with mental illnesses, neurological diseases, and head trauma because of the disruptive changes in brain activity that such issues can cause(1). For example, someone with chronic anxiety might have underactive alpha brain waves which strongly contribute to panic attacks and restlessness(2). Fortunately for us, our brains are adaptable. With enough neurofeedback training, our brains can correct the preexisting imbalances, form lasting positive changes, and significantly improve behavioral function.
Request More Information:

Incredibly safe, non-invasive therapy with no common side effects
Highly personalized therapy that creates lasting improvements up to years after therapy ends
Who Can Neurofeedback Help?
Neurofeedback can be used to reduce the symptoms of the following diseases and illnesses. A unique protocol is designed for each client depending on their symptoms, and it is adjusted as they progress through further sessions(1,2).
- Insomnia / Sleep Issues(29-33)
- Lyme Disease(34)
- Migraines and Headaches(35-38)
- Obsessive Compulsive Disorder(39-40)
- Performance Enhancement
- Post-COVID Syndrome(41)
- Post-Traumatic Stress Disorder(42-43)
- Social Anxiety Disorder(10-14)
- Traumatic Brain Injuries(44-47)
How Does Neurofeedback Work?
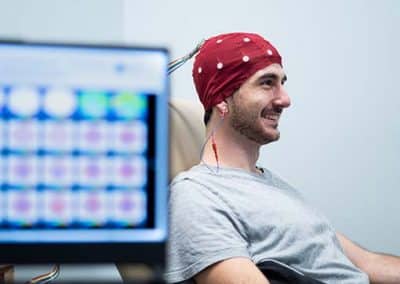
Neurofeedback works by monitoring your brain waves in real time and providing your brain with instant feedback. This “feedback” can take different forms depending on the person being treated. For example, a common practice is to have the client watch a movie during their session. Whenever the client’s brain waves are at the desired range, the movie plays in high quality (feedback). However, as soon as the client’s brain wave activity diverts from that optimal range, the movie starts to get blurry (more feedback).
The client’s brain starts to learn that, in order to get the movie to play in high quality, it must reach the desired pattern of brain wave activity. Your brain eventually learns to constantly function at the optimal pattern of activity as opposed to the unhealthy pattern at which it previously operated. This electrical changes in your brain are translated into real, visible behavioral improvements such as improved mood, decreased anxiety, and better cognitive functioning.
What Are the Benefits of Neurofeedback?
While the effects depend on the patient, condition being treated, number and frequency of of treatments. Patients who have received neurofeedback training have experienced the following benefits in as little as 10 sessions.
- Improved Memory
- Increased Focus
- Improved Self Regulation
- Better Manage Stress
- Improved Sleep
- Reduced ADHD Symptoms
- Reduced Anxiety
- Improved Depression Symptoms
Frequently Asked Questions About Neurofeedback
How do I get started with Neurofeedback (new patients)?
Before you come into the clinic, you will need to register as a patient in our patient portal. Here you will enter your medical history and primary reason/s for starting Neurofeedback. After this step, you will be able to schedule an initial consultation with our Nurse Practitioner. You will then need a Neurofeedback-specific consultation our Neurofeedback practitioner. This will include a more detailed conversation about how Neurofeedback can help you, as well as a brain map (quantitative EEG) to guide your Neurofeedback protocol development.
How do I add Neurofeedback to my treatment plan (existing patients)?
If you are already receiving treatment at Extivita (HBOT, nutritional IV’s, etc), you do not need to complete another consultation with our Nurse Practitioner. However, you will need a consultation with our Neurofeedback practitioner. This will include a more detailed conversation about how Neurofeedback can help you, as well as a brain map (quantitative EEG) to guide your Neurofeedback protocol development.
What happens in a Neurofeedback session?
How long does a Neurofeedback session last?
How often are Neurofeedback sessions?
What will my Neurofeedback protocol be?
How many Neurofeedback sessions will I need?
This depends on the condition that you are receiving Neurofeedback for, as well as how well your brain responds to training. In most cases, you should start to notice improvements after 10 sessions, although some patients may experience this earlier or later. We recommend 20 or more sessions to ensure that the improvements you make during training persist for months to years after you stop receiving Neurofeedback.
What is a brain map (qEEG)?
Is Neurofeedback safe?
Is anything being put into my brain?
Recent Neurofeedback News & Research
Neurofeedback: Optimize Brain Functioning
What is Neurofeedback? Neurofeedback, an innovative technology that enables individuals to observe and influence their brainwave activity, has emerged as a fascinating field at the forefront of neuroscience research. By providing real-time...
How hyperbaric oxygen therapy for depression gives you strength to heal
Mental Health | Published: March 1st 2022, 08:53AM Discover why the healing powers of oxygen are so beneficial for patients battling this increasingly common mood disorder Before the pandemic, depression was one of the leading mental health...
Is Neurofeedback an Effective Treatment for Depression?
Is Neurofeedback an Effective Treatment for Depression? Posted on: December 23rd, 2020 by NeuroHealth Associates Some people consider depression to be an ‘invisible’ disability. No one can see that you’re suffering because it all happens...
References:
- D. Corydon Hammond (2011) What is Neurofeedback: An Update, Journal of Neurotherapy, 15:4, 305-336, DOI: 10.1080/10874208.2011.623090
- Marzbani, Hengameh, et al. “Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications.” Basic and Clinical Neuroscience, vol. 7, no. 2, Apr. 2016, pp. 143–58. PubMed Central, doi:10.15412/J.BCN.03070208
- Luijmes, Robin E., et al. “The Effectiveness of Neurofeedback on Cognitive Functioning in Patients with Alzheimer’s Disease: Preliminary Results.” Neurophysiologie Clinique/Clinical Neurophysiology, vol. 46, no. 3, June 2016, pp. 179–87. ScienceDirect, doi:10.1016/j.neucli.2016.05.069.
- Surmeli, Tanju, et al. “Quantitative EEG Neurometric Analysis–Guided Neurofeedback Treatment in Dementia: 20 Cases. How Neurometric Analysis Is Important for the Treatment of Dementia and as a Biomarker?” Clinical EEG and Neuroscience, vol. 47, no. 2, SAGE Publications Inc, Apr. 2016, pp. 118–33. SAGE Journals, doi:10.1177/1550059415590750.
- Jang, Jung-Hee, et al. “Beta Wave Enhancement Neurofeedback Improves Cognitive Functions in Patients with Mild Cognitive Impairment.” Medicine, vol. 98, no. 50, Dec. 2019. PubMed Central, doi:10.1097/MD.0000000000018357.
- Lavy, Yotam, et al. “Neurofeedback Improves Memory and Peak Alpha Frequency in Individuals with Mild Cognitive Impairment.” Applied Psychophysiology and Biofeedback, vol. 44, no. 1, 2019, pp. 41–49. PubMed, doi:10.1007/s10484-018-9418-0.
- Marlats, Fabienne, et al. “SMR/Theta Neurofeedback Training Improves Cognitive Performance and EEG Activity in Elderly With Mild Cognitive Impairment: A Pilot Study.” Frontiers in Aging Neuroscience, vol. 12, June 2020. PubMed Central, doi:10.3389/fnagi.2020.00147.
- Angelakis, Efthymios, et al. “EEG Neurofeedback: A Brief Overview and an Example of Peak Alpha Frequency Training for Cognitive Enhancement in the Elderly.” The Clinical Neuropsychologist, vol. 21, no. 1, Jan. 2007, pp. 110–29. PubMed, doi:10.1080/13854040600744839.
- Becerra, Judith, et al. “Neurofeedback in Healthy Elderly Human Subjects with Electroencephalographic Risk for Cognitive Disorder.” Journal of Alzheimer’s Disease, vol. 28, no. 2, IOS Press, Jan. 2012, pp. 357–67. content.iospress.com, doi:10.3233/JAD-2011-111055.
- Hammond, D. Corydon. “Neurofeedback Treatment of Depression and Anxiety.” Journal of Adult Development, vol. 12, no. 2, Aug. 2005, pp. 131–37. Springer Link, doi:10.1007/s10804-005-7029-5.
- Biriukova, E. N., et al. “P.3.041 Clinical and Neurophysiological efficacy of Neurofeedback in the Combined Therapy of Anxiety Disorders Resistant to Psychopharmacotherapy.” European Neuropsychopharmacology, vol. 15, Jan. 2005, pp. S162–63. ScienceDirect, doi:10.1016/S0924-977X(05)80337-2.
- Dadashi, Mohsen, et al. “Effects of Increase in Amplitude of Occipital Alpha & Theta Brain Waves on Global Functioning Level of Patients with GAD.” Basic and Clinical Neuroscience, vol. 6, no. 1, Jan. 2015, pp. 14–20.
- Hou, Yue, et al. “Neurofeedback Training Improves Anxiety Trait and Depressive Symptom in GAD.” Brain and Behavior, vol. n/a, no. n/a, p. e02024. Wiley Online Library, doi:https://doi.org/10.1002/brb3.2024.
- Moscovitch, David A., et al. “Frontal EEG Asymmetry and Symptom Response to Cognitive Behavioral Therapy in Patients with Social Anxiety Disorder.” Biological Psychology, vol. 87, no. 3, July 2011, pp. 379–85. PubMed, doi:10.1016/j.biopsycho.2011.04.009.
- Enriquez-Geppert, Stefanie, et al. “Neurofeedback as a Treatment Intervention in ADHD: Current Evidence and Practice.” Current Psychiatry Reports, vol. 21, no. 6, 2019. PubMed Central, doi:10.1007/s11920-019-1021-4.
- González-Castro, Paloma, et al. “Efficacy of Neurofeedback Versus Pharmacological Support in Subjects with ADHD.” Applied Psychophysiology and Biofeedback, vol. 41, no. 1, Mar. 2016, pp. 17–25. Springer Link, doi:10.1007/s10484-015-9299-4.
- Van Doren, Jessica, et al. “Sustained Effects of Neurofeedback in ADHD: A Systematic Review and Meta-Analysis.” European Child & Adolescent Psychiatry, vol. 28, no. 3, Mar. 2019, pp. 293–305. Springer Link, doi:10.1007/s00787-018-1121-4.
- van Hoogdalem, Lothar E., et al. “The Effectiveness of Neurofeedback Therapy as an Alternative Treatment for Autism Spectrum Disorders in Children: A Systematic Review.” Journal of Psychophysiology, Hogrefe Publishing, 2020, p. No Pagination Specified-No Pagination Specified. APA PsycNET, doi:10.1027/0269-8803/a000265.
- Kouijzer, Mirjam E. J., et al. “Neurofeedback Treatment in Autism. Preliminary Findings in Behavioral, Cognitive, and Neurophysiological Functioning.” Research in Autism Spectrum Disorders, vol. 4, no. 3, July 2010, pp. 386–99. ScienceDirect, doi:10.1016/j.rasd.2009.10.007.
- Kouijzer, Mirjam E. J., et al. “Long-Term Effects of Neurofeedback Treatment in Autism.” Research in Autism Spectrum Disorders, vol. 3, no. 2, Apr. 2009, pp. 496–501. ScienceDirect, doi:10.1016/j.rasd.2008.10.003.
- Kouijzer, Mirjam E. J., et al. “Neurofeedback Improves Executive Functioning in Children with Autism Spectrum Disorders.” Research in Autism Spectrum Disorders, vol. 3, no. 1, Jan. 2009, pp. 145–62. ScienceDirect, doi:10.1016/j.rasd.2008.05.001.
- Pineda, J. A., et al. “Positive Behavioral and Electrophysiological Changes Following Neurofeedback Training in Children with Autism.” Research in Autism Spectrum Disorders, vol. 2, no. 3, July 2008, pp. 557–81. ScienceDirect, doi:10.1016/j.rasd.2007.12.003.
- Trambaiolli, Lucas, et al. “Neurofeedback Training in Major Depressive Disorder: A Systematic Review of Clinical Efficacy, Study Quality and Reporting Practices.” preprint, PsyArXiv, 1 Sept. 2020. DOI.org (Crossref), doi:10.31234/osf.io/5j4wy.
- Dias, Álvaro Machado, and Adrian van Deusen. “A New Neurofeedback Protocol for Depression.” The Spanish Journal of Psychology, vol. 14, no. 1, May 2011, pp. 374–84. DOI.org (Crossref), doi:10.5209/rev_SJOP.2011.v14.n1.34.
- Hammond, D. Corydon. “Neurofeedback Treatment of Depression and Anxiety.” Journal of Adult Development, vol. 12, no. 2, Aug. 2005, pp. 131–37. Springer Link, doi:10.1007/s10804-005-7029-5.
- Terrasa, Juan L., et al. “Self-Regulation of SMR Power Led to an Enhancement of Functional Connectivity of Somatomotor Cortices in Fibromyalgia Patients.” Frontiers in Neuroscience, vol. 14, Frontiers, 2020. Frontiers, doi:10.3389/fnins.2020.00236.
- Wu, Yu-Lin, et al. “Effects of Neurofeedback on Fibromyalgia: A Randomized Controlled Trial.” Pain Management Nursing, Feb. 2021. ScienceDirect, doi:10.1016/j.pmn.2021.01.004.
- Kayiran, Sadi, et al. “Neurofeedback Intervention in Fibromyalgia Syndrome; a Randomized, Controlled, Rater Blind Clinical Trial.” Applied Psychophysiology and Biofeedback, vol. 35, no. 4, Dec. 2010, pp. 293–302. PubMed, doi:10.1007/s10484-010-9135-9.
- Arns, Martijn, et al. “Differential Effects of Theta/Beta and SMR Neurofeedback in ADHD on Sleep Onset Latency.” Frontiers in Human Neuroscience, vol. 8, Dec. 2014. PubMed Central, doi:10.3389/fnhum.2014.01019.
- Schabus, Manuel, et al. “Enhancing Sleep Quality and Memory in Insomnia Using Instrumental Sensorimotor Rhythm Conditioning.” Biological Psychology, vol. 95, Jan. 2014, pp. 126–34. ScienceDirect, doi:10.1016/j.biopsycho.2013.02.020.
- Hammer, Barbara U., et al. “Neurofeedback for Insomnia: A Pilot Study of Z-Score SMR and Individualized Protocols.” Applied Psychophysiology and Biofeedback, vol. 36, no. 4, Dec. 2011, pp. 251–64. PubMed, doi:10.1007/s10484-011-9165-y.
- Cortoos, Aisha, et al. “An Exploratory Study on the Effects of Tele-Neurofeedback and Tele-Biofeedback on Objective and Subjective Sleep in Patients with Primary Insomnia.” Applied Psychophysiology and Biofeedback, vol. 35, no. 2, June 2010, pp. 125–34. DOI.org (Crossref), doi:10.1007/s10484-009-9116-z.
- Perlis, Michael L., et al. “Beta/Gamma EEG Activity in Patients with Primary and Secondary Insomnia and Good Sleeper Controls.” Sleep, vol. 24, no. 1, Jan. 2001, pp. 110–17. Silverchair, doi:10.1093/sleep/24.1.110.
- Brown, Valdeane. “Neurofeedback and Lyme’s Disease:” Journal of Neurotherapy, vol. 1, no. 2, Routledge, Aug. 1995, pp. 60–73. Taylor and Francis+NEJM, doi:10.1300/J184v01n02_05.
- Kosari, Zahra, et al. “Comparing the Effectiveness of Neurofeedback and Transcranial Direct Current Stimulation on Sleep Quality of Patients With Migraine.” Basic and Clinical Neuroscience, vol. 10, no. 6, 2019, pp. 579–88. PubMed Central, doi:10.32598/BCN.10.6.651.3.
- Walker, Jonathan E. “QEEG-Guided Neurofeedback for Recurrent Migraine Headaches.” Clinical EEG and Neuroscience, vol. 42, no. 1, SAGE Publications Inc, Jan. 2011, pp. 59–61. SAGE Journals, doi:10.1177/155005941104200112.
- Stokes, Deborah A., and Martha S. Lappin. “Neurofeedback and Biofeedback with 37 Migraineurs: A Clinical Outcome Study.” Behavioral and Brain Functions : BBF, vol. 6, Feb. 2010, p. 9. PubMed Central, doi:10.1186/1744-9081-6-9.
- Siniatchkin, M., et al. “Self-Regulation of Slow Cortical Potentials in Children with Migraine: An Exploratory Study.” Applied Psychophysiology and Biofeedback, vol. 25, no. 1, Mar. 2000, pp. 13–32. PubMed, doi:10.1023/a:1009581321624.
- Hammond, Corydon. “QEEG-Guided Neurofeedback in the Treatment of Obsessive Compulsive Disorder.” Journal of Neurotherapy, vol. 7, no. 2, Routledge, Mar. 2003, pp. 25–52. Taylor and Francis+NEJM, doi:10.1300/J184v07n02_03.
- Hammond, D. Corydon. “Neurofeedback with Anxiety and Affective Disorders.” Child and Adolescent Psychiatric Clinics of North America, vol. 14, no. 1, Jan. 2005, pp. 105–23, vii. PubMed, doi:10.1016/j.chc.2004.07.008.
- Luctkar-Flude, Marian, and Dianne Groll. “A Systematic Review of the Safety and Effect of Neurofeedback on Fatigue and Cognition.” Integrative Cancer Therapies, vol. 14, no. 4, SAGE Publications Inc STM, July 2015, pp. 318–40. SAGE Journals, doi:10.1177/1534735415572886.
- Kolk, Bessel A. van der, et al. “A Randomized Controlled Study of Neurofeedback for Chronic PTSD.” PLOS ONE, vol. 11, no. 12, Public Library of Science, Dec. 2016, p. e0166752. PLoS Journals, doi:10.1371/journal.pone.0166752.
- Reiter, Karen, et al. “Neurofeedback Treatment and Posttraumatic Stress Disorder: Effectiveness of Neurofeedback on Posttraumatic Stress Disorder and the Optimal Choice of Protocol.” The Journal of Nervous and Mental Disease, vol. 204, no. 2, Feb. 2016, pp. 69–77. journals.lww.com, doi:10.1097/NMD.0000000000000418.
- Bennett, Cathlyn N., et al. “Clinical and Biochemical Outcomes Following EEG Neurofeedback Training in Traumatic Brain Injury in the Context of Spontaneous Recovery.” Clinical EEG and Neuroscience, vol. 49, no. 6, Nov. 2018, pp. 433–40. PubMed, doi:10.1177/1550059417744899.
- Munivenkatappa, Ashok, et al. “EEG Neurofeedback Therapy: Can It Attenuate Brain Changes in TBI?” NeuroRehabilitation, vol. 35, no. 3, IOS Press, Jan. 2014, pp. 481–84. content.iospress.com, doi:10.3233/NRE-141140.
- Reddy, Rajakumari P, et al. “Neurofeedback Training to Enhance Learning and Memory in Patient with Traumatic Brain Injury: A Single Case Study.” The Indian Journal of Neurotrauma, vol. 6, no. 1, June 2009, pp. 87–90. ScienceDirect, doi:10.1016/S0973-0508(09)80037-3.
- Reddy, Rajakumari Pampa, et al. “Silent Epidemic: The Effects of Neurofeedback on Quality-of-Life.” Indian Journal of Psychological Medicine, vol. 36, no. 1, 2014, pp. 40–44. PubMed Central, doi:10.4103/0253-7176.127246.